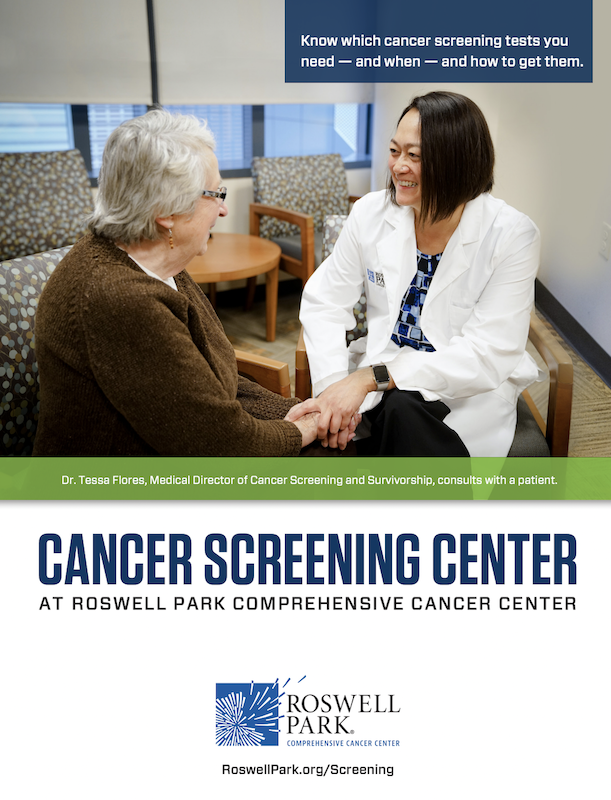
Have questions about which screenings and when, or what other factors may affect your risk?
We can help. Take our quiz to learn which cancer screenings you need now.
Get Screened
If you know you’re due for a cancer screening, schedule it today! Roswell Park offers screening programs for lung cancer and breast cancer at both our downtown and select Roswell Park Care Network locations. To determine your eligibility for those programs, click below.
Schedule a lung cancer screening Schedule a mammogram
Screenings for other types of cancers, including cervical, colorectal and early detection of prostate cancer, can be arranged through your primary care or other specialists. If you’re not sure of your screening needs, take our quiz to get started.
Stay Informed
How often do you need a colonoscopy? When should you begin mammograms? Download our info sheet to stay on track.
Know your risk
Learn which cancer screenings are right for you, based on age, gender and family history.
By disease
- Age 40 and older should have annual breast cancer screening with mammography along with clinical exams.
- Younger than age 40 should discuss their personal risk factors, and medical and family history with their physician to determine when to begin annual mammography screening.
- With major risk factors, including a strong family history or a known mutation in a gene associated with breast cancer, should begin yearly screening before age 40. Because breast cancer in younger women is harder to detect with mammography, women should speak with their doctor about whether other screening tests such as magnetic resonance imaging (MRI) are advised.
- All women should begin cervical cancer screening at age 21.
- Women between the ages of 21 and 29 should have a Pap test every 3 years. They should not be tested for HPV unless it is needed after an abnormal Pap test result.
- Women between the ages of 30 and 65 should have both a Pap test and an HPV test every 5 years. This is the preferred approach, but it is also acceptable to have a Pap test alone every 3 years.
- Women over age 65 who have had regular screenings with normal results should not be screened for cervical cancer. Women who have been diagnosed with cervical pre-cancer should continue to be screened.
- Women who have had their uterus and cervix removed in a hysterectomy and have no history of cervical cancer or pre-cancer should not be screened.
- Women who have had the HPV vaccine should still follow the screening recommendations for their age group.
- Women who are at high risk for cervical cancer may need to be screened more often. Women at high risk might include those with HIV infection, organ transplant, or exposure to the drug DES. These women should consult with their doctor or nurse.
- Colon cancer is largely preventable, but you must have a screening test that will detect warning signs such as polyps, abnormal growths, precancerous lesions or early malignancies, long before you notice any symptoms.
- All adults should begin screening for colon and rectal cancer at age 45 unless other risk factors or symptoms indicate screening should begin at an earlier age.
You should be screened if:
- History of cancer of the lung, esophagus, head or neck (excluding cancer of the thyroid)
or - These three factors:
- Age 50 to 79
- 20 Pack/Years of smoking history
- Smoked within the past 15 years
Other risk factors will be considered in determining your screening needs, such as:
- Asbestos-related lung disease or pulmonary asbestosis
- History of emphysema
- Chronic obstructive pulmonary disease (COPD)
- Family history of lung cancer (parent, sibling or child)
- Two or more first-degree relatives (parent, sibling or child) who were diagnosed with pancreatic cancer
- Three or more blood relatives, with at least one affected first-degree relative who were diagnosed with pancreatic cancer
- A diagnosis of Peutz-Jeghers syndrome (associated with mutations in the STK11 gene)
- Genetic Testing showing a genetic mutation of BRCA2 and you have two family members (or one first-degree relative) diagnosed with pancreatic cancer
- Genetic testing that shows a genetic syndrome or mutation that increases risk for pancreatic cancer, such as Lynch syndrome, Familial Atypical Multiple Mole Melanoma (FAMMM) syndrome, or mutation of P16 or PALB2, and you have a first-degree relative with pancreatic cancer.
- You are African-American
- You have a father or brother who had prostate cancer — especially if they were younger than 60 at the time of diagnosis
- You have undergone genetic screening that showed you have a genetic mutation (such as BRCA1, BRCA2, ATM, HOXB13, MLH1, MSH2 or MSH6)
If you have a family history of prostate cancer, you should talk with your doctor about beginning early-detection testing 10 years before the age of the earliest prostate cancer case in your family (for example, at age 35 if your father or brother received a prostate cancer diagnosis at age 45).
If you do not fall into any of the groups above, you may consider beginning early detection with baseline PSA test and digital rectal exam at age 45.
A PSA test is generally not recommended for men 70 and older unless they are very healthy and have a life expectancy of 10 years or more.
Screening for first responders
First responders face unique occupational health risks. Find out how significant your cancer risk is.

Please, please let my sister be your inspiration for practicing sun safety, getting your skin checked, learning the risk factors and living life to the fullest.
Indigenous & Rural Patient Navigation Program
Cancer care is not an easy journey, but we can help clear the path and walk alongside you. Our Indigenous & Rural Patient Navigation Program is a free, non-clinical service to help you get the cancer care you need — from cancer screenings to survivorship services.
“Early detection and persistence saved my life. This experience made me a more humble, caring, new person.”
“I thought of my father and brothers and decided it would be good to know where I stood right now. I got tested early and it saved my life.”
“Staying on top of your checkups and taking advantage of these screenings can literally save your life. If sharing my story will encourage someone to get checked, then I’m happy to do it.”