Roswell Park’s speech-language pathologists provide a variety of services to help you overcome speech, language, voice, swallowing, and hearing problems following cancer treatment.
While undergoing cancer treatments, such as surgery, chemotherapy, and radiation therapy, your ability to swallow, speak, or communicate may be affected. Our speech-language pathologists have extensive training in diagnostics and therapy in the areas of swallowing, speech, language, voice therapy and alaryngeal speech, to provide assessment and treatment for both outpatients and inpatients at Roswell Park.
Patients with all types of cancers may experience symptoms that require treatment from a speech-language pathologist. They are, however, most often seen in patients undergoing:
- Treatment for cancers of the head and neck
- Treatment for cancers of the lungs or esophagus
- Treatment for brain tumors, including neurosurgery and neuro-oncology
- Services for patients who have spent time in the ICU or IMCU
As an NCI-designated cancer center, we have expertise in cancer-related speech, language, voice and swallowing disorders – as well as access to the latest technologies, therapeutic and diagnostic tools that allow us to offer highly precise evaluations and innovative therapeutic options.
Swallowing therapy
A modified barium swallow exam (also called videofluoroscopy or video cervical esophagram) is a video technology, similar to an x-ray. During the exam, a patient swallows various consistencies of food, ranging from liquids to solids, that contain a substance called barium, allowing the food or liquid to be visualized on the x-ray.
By watching the swallowing process on the x-ray, our team can identify problems the patient may be having, test strategies to compensate for them, and make a plan of care specific to the patient’s needs.
During a flexible endoscopic evaluation (FEES), sometimes called a fiber-optic endoscopic evaluation, a thin, flexible tube called an endoscope is inserted through the patient’s nose and guided into the throat. A camera and light source at the tip of the tube allow the speech-language pathologist (SLP) to visualize the anatomy in the throat. The patient is given various consistencies to swallow, allowing the SLP to evaluate swallowing function, airway protection, and rule out aspiration.
The SLP will evaluate the patient before treatment, midway through, and upon completion of treatment — patients identified as having a swallowing impairment are seen for swallowing therapy post-treatment.
During these therapy sessions, the SLP will:
- Teach the patient exercises to stretch and strengthen the muscles involved in swallowing.
- Assess for changes in the ability to swallow as the patient goes through radiation therapy.
- Help the patient to maintain ability to swallow after treatment is done to prevent long-term or late-onset changes.
Some patients may experience the following side effects that impact swallowing function while undergoing radiation treatment. Our speech-language pathologists will work with patients to help manage:
- Pain when swallowing (odynophagia)
- Sores (mucositis) in the mouth and throat
- Changes in salivary flow including thick secretions and dry mouth (xerostomia)
- Swelling or lymphedema of the oral cavity, pharynx, and larynx
- Changes in taste
- Trismus, a condition where the muscles of the jaw become contracted and sometimes inflamed, preventing the mouth from fully opening.
- Aspiration or the accidental ingestion of a fluid or solid into the trachea (windpipe) and lungs. When food or liquids "go down the wrong pipe," you are experiencing aspiration.
Speech & voice therapy
When treating head and neck cancers, Roswell Park surgeons and oncologists use specialized techniques and approaches to preserve your speech and communication function as much as possible. Our speech pathology team works closely with patients to help preserve and improve speech function before and after treatment.
As a result of treatment, a patient may develop weakness, reduced range of motion or lack of coordination in tongue, lips, cheeks, and other muscles you use to help you form words to create speech. The speech pathology team can offer a range of exercises, strategies, and techniques to help you speak more clearly.
If a patient requires a prosthetic device as part of reconstruction following surgery for oral cancer, we will work closely with our specialized dental team to help ensure the device is functional to meet the patient’s needs, as well as providing therapy to complement the use of the prosthetic.
A patient may develop problems with his or her voice as a result of cancer or its treatment. Surgery or radiation therapy may cause the voice to become hoarse, weak, or completely lost. Additionally, a tumor or lesion itself may affect the mobility of the vocal cords and quality of the voice.
Our SLP team provides voice evaluations, including analyses of vocal fold function and voice production. We use a technology called video laryngoscopy that provides a real time view of the vocal folds. This painless, noninvasive procedure uses an endoscope to capture real time movement of the vocal cords and still images that are used to create a treatment plan to best address the patient’s specific areas of deficit.
Voice therapy uses a number of techniques to compensate for an affected vocal fold. This may include exercises, biofeedback techniques, and certain devices to increase and maximize muscle strength in your vocal folds, as well as to improve breath support for the voice and decrease vocal strain.
In some cases of benign vocal fold lesions, voice therapy alone may improve the symptoms, allowing the patient to avoid surgery. Other times, voice therapy plays a key role after surgery to improve healing and prevent recurrent damage to the vocal cords.
Laryngectomy is a surgery performed to remove the larynx (voice box). If the larynx is removed, the patient will need to learn a new way to communicate as part of recovery. Our speech-language pathology team has expertise in working with laryngectomees to regain their ability to communicate after surgery.
The SLPs provide comprehensive rehabilitation and counseling regarding changes to communication before and after surgery, and work closely with the patient and their family throughout the recovery process.
Electrolarynx
An electronic larynx (electrolarynx), is a battery operated machine that produces sound for the patient to create a voice. Using the electrolarynx as a sound source, the patient is able to move the muscles in their mouth to create speech. Many patients can use the device within three to five days after surgery, initially using an adaptor for the mouth.
Esophageal speech
This approach to voicing after laryngectomy uses the esophagus as the sound source for speech. It involves swallowing or injecting air into the esophagus and then pushing it back up through the throat and mouth, to vibrate the esophagus and serve as a sound source for speech production.
Tracheoesophageal (TEP) speech
This is another way of communication in which the esophagus serves as the sound source to create speech. In order to enable TEP speech, the head & neck surgeon creates a small opening between the esophagus and the trachea (windpipe) and places a small one-way valve in the newly created tract. This procedure is called tracheoesophageal puncture. The one-way valve keeps food out of your windpipe but allows air to be injected into the esophagus to serve as a sound source for the patient to achieve voicing.
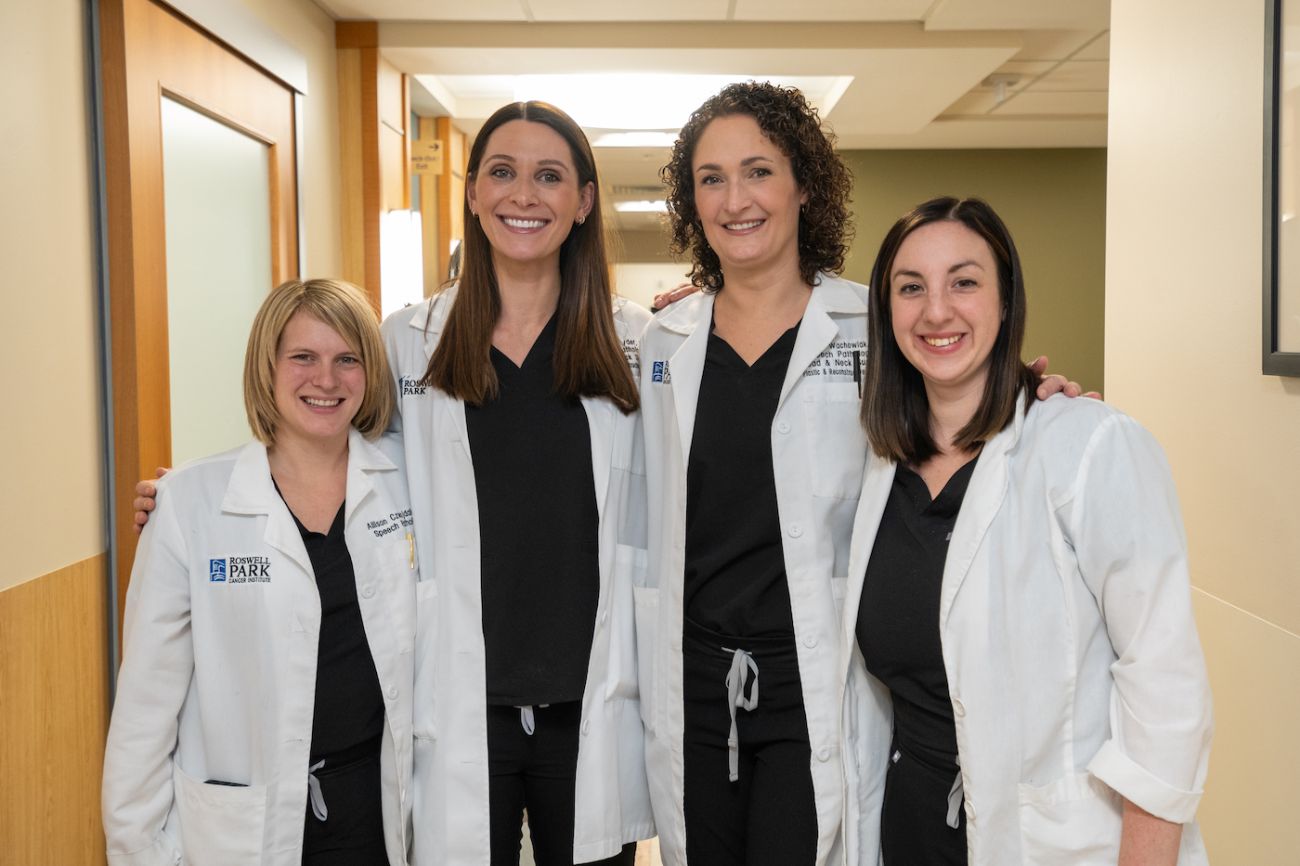
Meet the team
Lindsay Wachowiak MA, CCC-SLP
Supervising Speech-Language Pathologist
Lauren Snyder MS, CCC-SLP
Speech-Language Pathologist
Sarah Crance MS, CCC-SLP
Speech-Language Pathologist
Allison Czwojdak MA, CCC-SLP
Speech-Language Pathologist