A pioneering approach that discovers features of your cancer that make it treatable with new cancer therapies.
Theranostics employs methods and tools of diagnostic testing to deliver advanced cancer therapies. For decades, diagnostic tests have used radiopharmaceuticals, or radioactive drugs, most commonly as tracers for imaging scans of the heart, lung, kidneys, gallbladder and thyroid, and in treating thyroid conditions.
For example, with a typical positron emission tomography (PET) scan, patients receive an injection of a safe radioactive chemical as a tracer. Because cancerous cells absorb greater amounts of the tracer than healthy cells do, the scanner produces images that show where the cancer cells are in the body.
Theranostics builds on this by adding a radioactive component to new targeted therapy drugs that target specific unique features of a person’s cancer cells.
How it works
It began with thyroid treatment
Theranostics emerged from the success in treating thyroid conditions with radioactive iodine. Because the thyroid gland absorbs nearly all the iodine in the body, physicians determined that they could give patients a radioactive version of iodine that would concentrate in the thyroid and destroy diseased thyroid tissue.
Theranostics involves a two-step process, and all procedures are done as outpatient services.
Step 1. Diagnosis — Do your cancer cells have the target?
During a diagnostic scan, physicians use a special tracer that is a radioactive version of a targeted drug that targets a specific, unique marker (such as a protein) that may be found on the cancer cells. The drug finds cells with the target and binds to them while the radioactive component highlights them on the imaging — confirming that your cancer cells have the target.
Step 2. Therapy — Drugs deliver radiation directly to the cells
Then, the same (or similar) targeted drug, now carrying a stronger, treatment-level dose of radiation is delivered by an infusion or injection. The drug finds and binds to the cancer cells — anywhere in the body — delivering radiation directly to the individual cells, destroying them. Healthy cells without the specific target are left unharmed.
Cancers we treat
Roswell Park currently offers theranostic approaches for treating patients with these cancers:
Newly FDA approved, the drug Lutetium 177 vipivotide tetraxetan PSMA therapy (Pluvicto), treats patients with metastatic prostate cancer with cells that have a marker called prostate-specific membrane antigen (PSMA). Patients receive an infusion every six weeks for a total of six treatments.
Lutetium 177 dotatate (Lutathera) is used to treat patients with certain neuroendocrine tumors that have cells with proteins called somatostatin receptors. Lu 177 dotatate has been a game-changer for treating gastrointestinal neuroendocrine tumors. Patients typically receive a treatment infusion every eight weeks for a total of four doses.
Specifically for the rare tumor types of adult pheochromocytoma and paraganglioma, iobenguane Iodine 131/ MIBG (Azedra) is used to treat tumors that have a marker called norepinephrine transporter on the cells.
Theranostic treatments are well tolerated and take only minutes, followed by a period of observation. Patients go home the same day and radiation is eliminated through body fluids within days.
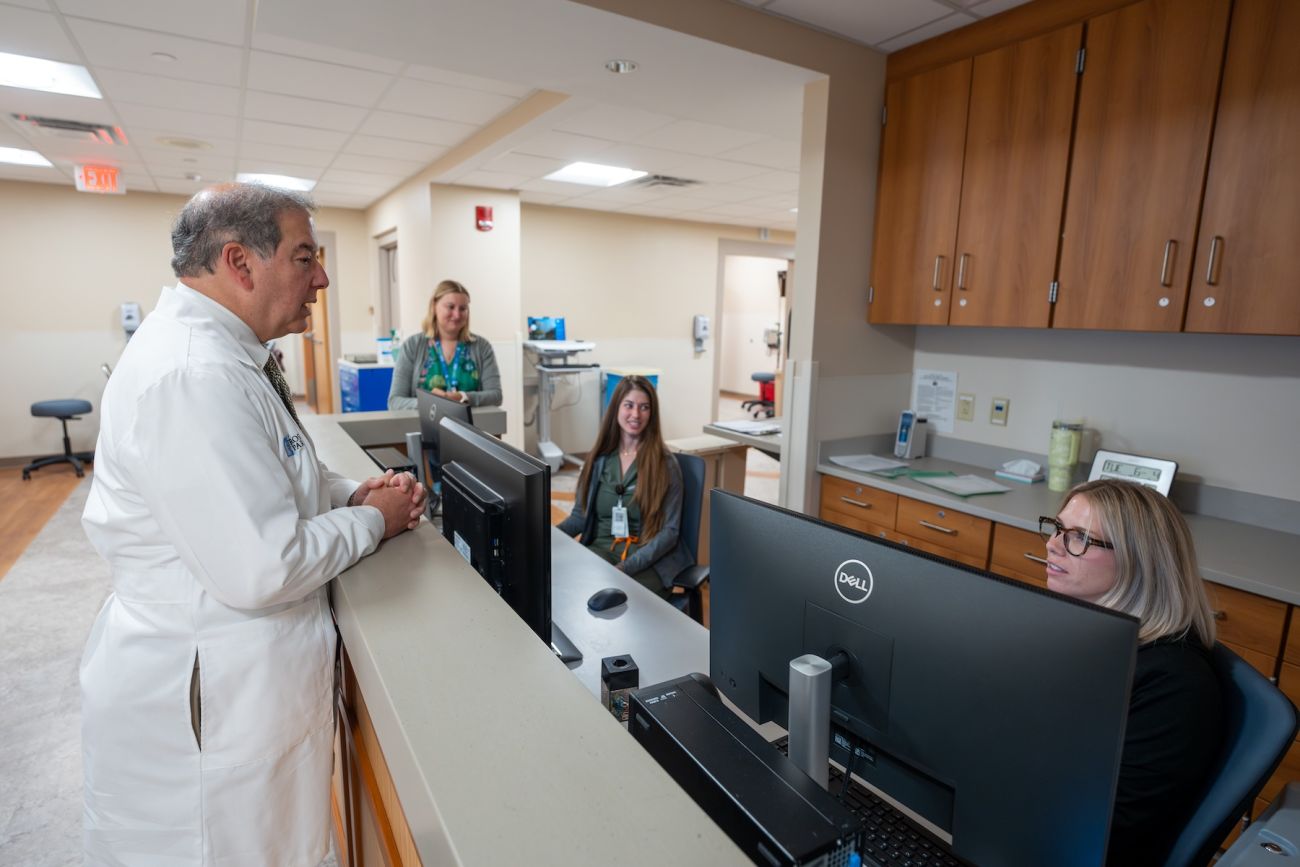
Why Roswell Park’s Theranostic Center
- We are among the few cancer centers in the nation with a dedicated theranostics program and we are building a new facility to expand our clinical space and greatly increase the number of patients we can accommodate.
- New suite of 4 shielded rooms dedicated to theranostic procedures
- Our experience from treating patients with Lutathera and Azedra, and clinical trials of Pluvicto.
As new diagnostic and therapeutic agents emerge, Roswell Park’s clinical trials program will continue to offer early access to these latest options.