Advancing care for patients with oral, head and neck cancers
Roswell Park Comprehensive Cancer Center has a long and illustrious history of providing dental, oral and maxillofacial services to cancer patients, particularly those affected by oral and head and neck cancers.
Building on this rich background of patient care, the Department of Oral Oncology was created in 2018 to integrate specialized clinical treatment with innovative research.
- 1968: Department of Dentistry and Maxillofacial Prosthetics established at Roswell Park with Dr. Norm Schaaf as the Chair.
- 1987: Dental Oncology Residency Program established
- 2018: Department of Oral Oncology created with Dr. Mukund Seshadri as the Chair
- 2018-2021: Five faculty members, three research fellows, six residents, seven graduate students
- 2018-2021: 26 peer-reviewed publications, ~$6.75M in research funding
What we do
The Oral Oncology department is the academic home for an integrated team of basic and translational scientists and clinicians who work closely to translate novel discoveries from the laboratory bench to the clinical setting.
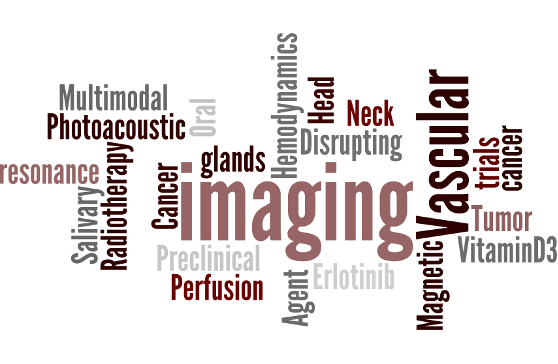
Our research programs focus on:
- Understanding the complex biology of oral cancers and how they resist treatment
- Developing novel preventative measures and treatment options
- Mitigating oral side effects of chemotherapy and radiation
- Developing new diagnostic/imaging methods for early detection of these esthetically and functionally debilitating cancers.
Ongoing research projects are funded by the National Cancer Institute (NCI), the National Institute for Dental and Craniofacial Research (NIDCR) and the Roswell Park Alliance Foundation.
Research highlights
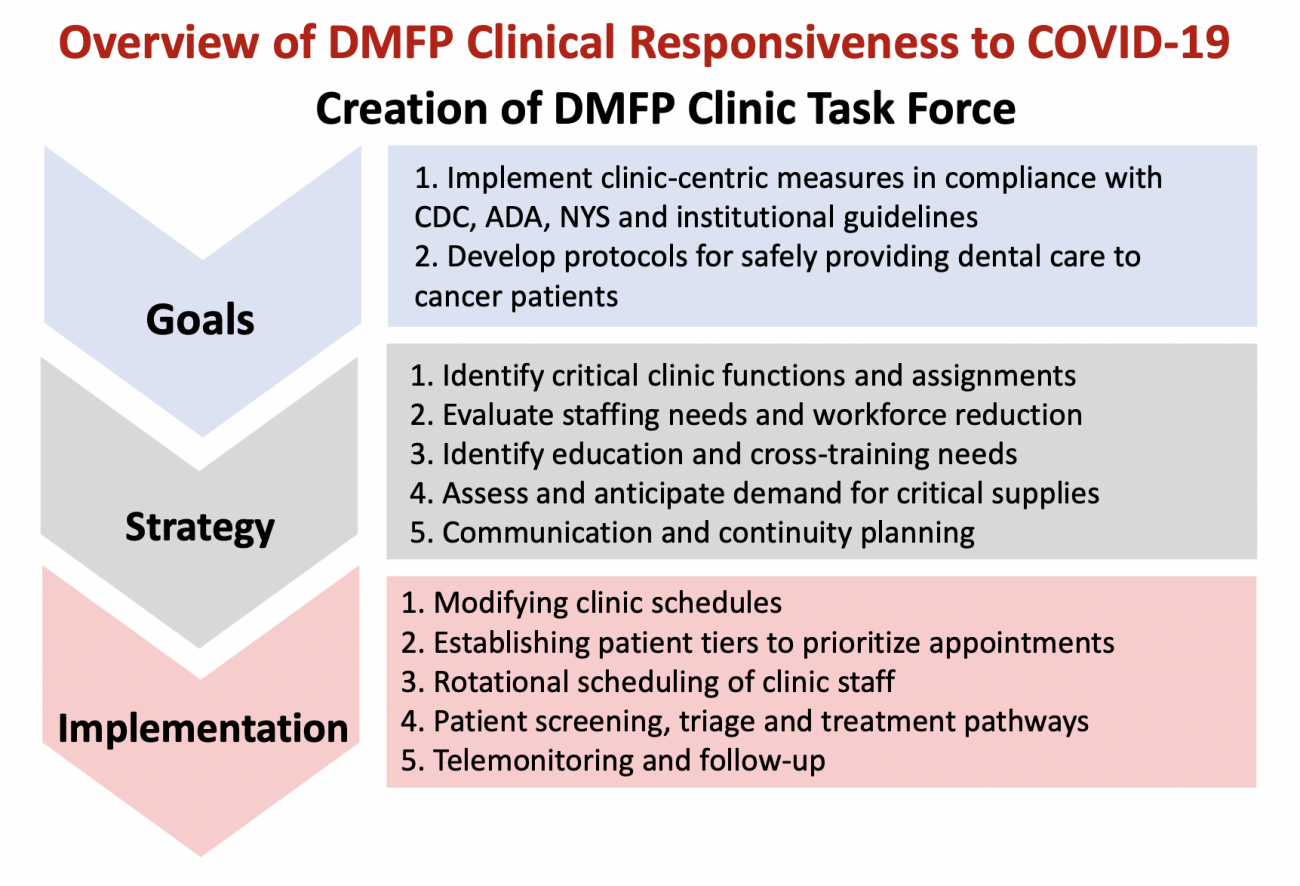
The outbreak of COVID-19 has changed all of our lives in a fundamental manner. Cancer patients, in particular, are often immunocompromised, rendering them susceptible to oral and respiratory infections including COVID-19.
Ongoing work in the Oral Oncology department is examining the impact of COVID-19 on oral cancer care and patient experience at Roswell Park. Researchers will assess how delays in care have affected high-risk cancer patients and survivors, including oral health complications related to cancer treatment.
Our scientists are also studying the acceptance and potential of tele-dentistry for monitoring and managing the oral healthcare needs of cancer patients and survivors.
Read more:
- Manuballa S, Abdelmaseh M, Tasgaonkar N, Frias V, Hess M, Crow H, Andreana S, Gupta V, Wooten KE, Markiewicz MR, Singh AK, Hicks WL Jr, Seshadri M. Managing the Oral Health of Cancer Patients During the COVID-19 Pandemic: Perspective of a Dental Clinic in a Cancer Center. J Clin Med. 2020 Sep 28;9(10):3138. doi: 10.3390/jcm9103138. PMID: 32998403; PMCID: PMC7600784.
Oral cancers are aggressive malignancies that lead to debilitating changes in speech, appearance and function in patients. Sadly, despite the mouth being readily accessible, most patients present with advanced disease at initial diagnosis.
Conventional examination of the mouth under white light is often insufficient to detect these cancers at an early stage. Development of early detection strategies can therefore have a tremendous impact on patient survival.
Our research focuses on developing and applying machine learning and artificial intelligence (AI) based analysis to MRI and US methods for detection of oral cancers at an earlier stage.
Read more:
- Panta P, Rich LJ, Seshadri M (2019). Advanced optical imaging methods in oral oncology. In: PantaP. (eds) Oral Cancer Detection. Springer, Cham. pp 189-204. 10.1007/978-3-319-61255-3_9.
- DeJohn CR, Seshadri M. Ultra-high frequency ultrasound as a clinical adjunct for imaging the oral cavity: added value of quantitative analysis. Dentomaxillofac Radiol. 2020 Oct;49(7):20200314. doi: 10.1259/dmfr.20200314. PMID: 32959693; PMCID: PMC7549526.
Since 2016, we’ve been studying the role of diet and dietary supplements, such as vitamin D, in oral cancer. We’ve shown that vitamin D deficiency can accelerate progression of oral cancer, while precise and controlled dietary supplementation of vitamin D to correct this deficiency can prevent development and progression of oral cancer.
Our findings suggest the need for a “precision medicine” approach to fully realize the benefit of vitamin D through tailored dietary supplementation regimens to patients based on their vitamin D levels.
Ongoing studies are focused on understanding how vitamin D levels in oral and head and neck cancer patients affect their response to treatment. We are also studying if/how vitamin D supplementation can enhance the immune system in oral cancer patients.
Read more:
- Vincent-Chong VK, DeJong H, Attwood K, Hershberger PA, Seshadri M. Preclinical Prevention Trial of Calcitriol: Impact of Stage of Intervention and Duration of Treatment on Oral Carcinogenesis. Neoplasia. 2019 Mar 12;21(4):376-388. PMID: 30875566; PMCID: PMC6416727.
- Verma A, Vincent-Chong VK, DeJong H, Hershberger PA, Seshadri M. Impact of dietary vitamin D on initiation and progression of oral cancer. J Steroid Biochem Mol Biol. 2020 Jan 22;199:105603. [Epub ahead of print] PMID: 31981799
Radiation therapy (RT) is an integral part of the management of head and neck cancer patients. However, most tumors resist radiation therapy. In addition, a majority of cancer patients who undergo radiation treatment are affected by severe dry mouth (xerostomia) and mucositis due to radiation damage to glands and normal oral tissues, which in turn predisposes them to oral infections.
We’re developing and testing novel imaging methods to better understand how head and neck tumors and surrounding normal tissues (for example, salivary glands) respond to radiation. Specifically, we have been testing the potential of ultrasound (US) and photoacoustic imaging (PAI) methods to map early changes in salivary glands following radiation.
These studies will help developing strategies that can not only improve the response of tumors to radiation (“radiosensitization”) but also protect salivary glands (“radioprotectors”) or accelerate their repair after radiation damage thereby mitigating the adverse consequences of radiation in cancer patients.
Read more:
- Rich LJ, Seshadri M. Photoacoustic monitoring of tumor and normal tissue response to radiation. Sci Rep. 2016 Feb 17;6:21237. doi: 10.1038/srep21237. PMID: 26883660; PMCID: PMC4756329.
- Rich LJ, Miller A, Singh AK, Seshadri M. Photoacoustic Imaging as an Early Biomarker of Radio Therapeutic Efficacy in Head and Neck Cancer. Theranostics. 2018 Mar 6;8(8):2064-2078. doi: 10.7150/thno.21708. PMID: 29721063; PMCID: PMC5928871.
- Rich LJ, Chamberlain SR, Falcone DR, Bruce R, Heinmiller A, Xia J, Seshadri M. Performance Characteristics of Photoacoustic Imaging Probes with Varying Frequencies and Light-delivery Schemes. Ultrason Imaging. 2019 Nov;41(6):319-335. doi: 10.1177/0161734619879043. Epub 2019 Sep 30. PMID: 31570083; PMCID: PMC7042667.
- Rich LJ, Bolookat ER, Seshadri M. Dynamic photoacoustic imaging of neurovascular coupling in salivary glands. J Oral Biosci. 2019 Dec;61(4):236-241. doi: 10.1016/j.job.2019.08.002. Epub 2019 Sep 3. PMID: 31491491; PMCID: PMC6910936.
Training the next generation of scientists
In addition to our research and community outreach, the Department of Oral Oncology is actively involved in hands-on teaching with Master’s and PhD candidates and medical students in our highly competitive graduate studies program.
Our multidisciplinary education model allows students a unique immersive experience, preparing them for successful careers as independent investigators.
Unmatched expertise
Research interests: Oral oncology; oral and maxillofacial radiology and radiobiology of head and neck cancers
Spotlight: Recent accomplishments
- In August 2022, the new 12,600 sq ft Head & Neck Surgery, Plastic Surgery, Speech Pathology & Dental Center opened on the third floor of the Main Hospital.
- In December 2020, Dr. Seshadri received a five-year, $2.9M R01 award from the National Cancer Institute (NCI) to develop clinically relevant models of head and neck cancer and test the efficacy of novel agents and FDA-approved non cancer drugs against these aggressive cancers.
- Dr. Vincent-Chong, a post-doctoral fellow in the Department of Oral Oncology, presented at the virtual meeting of the Oncology Models Forum, organized by the National Cancer Institute (NCI), in March 2021.
- PhD candidates Aparajita Verma and Eftekhar Rajab Bolookat presented their research at the AACR Virtual Special Conference: Radiation Science and Medicine in March 2021.
Contact us
Jessica McNamee
Associate Research Administrator
Phone: 716-845-1300 ext. 2523
Email: Jessica.McNamee@RoswellPark.org
Bruce Specht
Senior Executive Director
Department Administrator - Oral Oncology
Phone: 716-845-1065
Fax: 716-845-3944
Email: Bruce.Specht@RoswellPark.org