We know the last few years have been difficult and filled with even more distractions. But the time has come to get back on track for routine cancer screening and early detection practices, especially for people who are considered at higher-than-average risk for developing certain kinds of cancers.
In general, you could be considered at higher risk if you have a family history of certain cancers or if you have a known genetic mutation or abnormality associated with a predisposition for developing cancer, such as mutations to the BRCA1 or BRCA2 genes. While these are most commonly associated with breast cancer, BRCA mutations increase the risk of other cancers as well.
Here’s what experts from Roswell Park Comprehensive Cancer Center advise for cancer screening and early detection practices.
Breast cancer screening
“There are lots of things that can make you higher-risk for breast cancer,” says Jessica Young, MD, FACS, Director of the Breast Cancer Risk Assessment and Prevention Program at Roswell Park. “Having a strong family history or a known gene mutation, having previous biopsies of the breast especially if they show atypical cells, or having previous chest radiation for lymphoma are the big ones. There are other smaller factors too that, when combined, can give you an increased risk, such as not having children or having children later in life, taking hormone replacement therapy and other factors.”
Having a relative with other types of cancer, including ovarian or multiple types of cancer, can increase your risk of having a gene mutation that can put you at higher risk for breast cancer.
If there’s a family history of breast, ovarian or other cancer, doctors might recommend getting a mammogram earlier than 40, which is the age recommended for most women to get their first baseline mammogram. But it’s important to discuss family history with a primary care doctor or gynecologist in order to start establishing risk, she says. “Screening typically starts at age 40, or 10 years before the first person in the family was diagnosed with breast cancer, but no younger than 25. If you know you have a gene mutation it might influence when screening should begin. For people with BRCA mutations, it would start at age 25.”
High Risk Breast Cancer Screening Program Risk Level Assessment Form
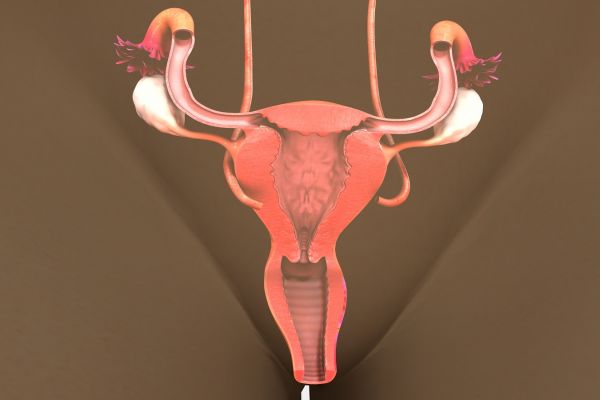
Ovarian cancer screening
Similar to breast cancer, women with a family history of breast or ovarian cancer might be considered higher-risk for developing ovarian cancer, as are those women who have a BRCA1 or BRCA2 mutation or have a family history of ovarian cancer, says Emese Zsiros, MD, PhD, FACOG, Chair of the Department of Gynecologic Oncology and Director of Research in the Department of Gynecologic Oncology at Roswell Park. Women who have struggled with endometriosis or who have Lynch syndrome, otherwise known as hereditary nonpolyposis colon cancer, might also be considered high risk.
The best way to confirm if you face a higher risk of developing ovarian cancer is to talk with a doctor and be genetically screened for mutations, Dr. Zsiros says. “Generally, this is done on a patient with cancer and, if they test positive for a genetic mutation, cascade testing is done on other members of their family.” Talking with a primary care physician or specialist can help determine whether that testing is needed and when.
“Once a patient is diagnosed as high risk, screening starts at age 30 until it is time for their risk-reducing surgery,” Dr. Zsiros says. “There are two screening tools currently available that we can provide: A serial blood test, CA-125, and a pelvic ultrasound every six months. Since these are the only screening methods available, we use them for high-risk patients until it’s time for surgery.” A risk-reducing surgery called a bilateral salpingo-oophorectomy, which involves removing both fallopian tubes and ovaries, might be recommended for a high-risk patient, based on national guidelines and the patient’s specific diagnosis and family history.
“If a patient is not considered high-risk but they are experiencing symptoms such as abdominal pain and bloating, unintentional weight loss, early satiety, new onset constipation, abdominal distention, nausea or vomiting and fatigue that persists over the course of three to four weeks, they should see a doctor right away.”
High Risk Ovarian Cancer Clinic Risk Level Assessment Form
Lung cancer screening
People considered high risk for developing lung cancer are adults aged 50 and older who smoked for at least 20 years, says Mary Reid, MSPH, PhD, Chief of Cancer Screening, Survivorship and Mentorship at Roswell Park. That’s the threshold for getting a low-dose CT, a kind of chest imaging that’s more sensitive than a standard x-ray and can help determine whether lung cancer is present.
“If you add on other factors, people can be considered to have a higher risk,” Dr. Reid says. “The more you smoked, in terms of packs per day and years. The older you are, if you have a family history of lung cancer, if you have any kind of obstructive respiratory disease, all of those factors increase your risk considerably. If you have a job where you breathe in fine particles, like being a firefighter, you’re likely at an increased risk for respiratory disease and lung cancer in general.”
If someone is younger than 50, or hasn’t smoked for 20 years, but they are symptomatic, they might be eligible for a low-dose CT or an x-ray, Dr. Reid says. Symptoms include a persistent cough, increased shortness of breath or the presence of blood in the sputum (or phlegm) after a hacking cough. Anyone with those symptoms should consult their primary care physician right away.
"Unfortunately, unlike breast or prostate cancer, not many people who are eligible for annual lung screens are getting them," Dr. Reid says. "That might be due to a sense of shame or guilt some tobacco users might feel, a sense that they somehow deserved it or brought it on. It’s a sense of judgment that doesn’t apply to any other type of health ailment and should no longer be applied to smokers.
"We need to be enthusiastic about lung cancer screening. This can save a person’s life. Lung cancer screening is the most effective test. If you have a colonoscopy and you have polyps removed, that process of screening and colonoscopy reduces colon cancer mortality by 50%. Lung cancer screening, getting a low-dose CT, reduces mortality over 20% more than just getting a chest scan alone. There are more lung cancer deaths than breast, pancreas and colorectal cancer combined. The impact on us as a society will be most greatly served if we screened the most eligible people for lung cancer.”
High Risk Lung Cancer Screening Program Risk Level Assessment Form
Pancreatic cancer screening
Pancreatic cancer is still an uncommon cancer but a person might be at high risk for developing it if they have a strong family history, the presence of certain precancerous conditions on their pancreas or genetic predisposition syndromes, including Peutz-Jeghers syndrome, hereditary pancreatitis, Lynch syndrome or BRCA 1/2 syndrome, says Christos Fountzilas, MD, FACP, a medical oncologist specializing in gastrointestinal cancers at Roswell Park. Peutz-Jeghers syndrome is an inherited condition in which unusual polyps and dark-colored spots develop in the digestive tract. People with this syndrome are at increased risk for pancreatic cancer as well as breast, colon, stomach, testicular, ovarian, lung, cervical and other types of cancer.
Another condition that could increase your risk is the development of intraductal papillary mucinous neoplasm (IPMN), a benign tumor that might, over time, become cancerous. These might be found during a CT completed for other reasons, such as for kidney stones. Upon further examination possibly including a biopsy, it is determined whether they are benign or if there is a need for immediate surgery. Your doctor may monitor IPMNs to see whether they continue to grow or become cancerous, at which point surgery would be an option.
“For screening, we’re looking at someone who has more than a 5% lifetime risk of developing pancreatic cancer. Having a syndrome doesn’t automatically mean you have an increased risk for cancer; it might be around 5%. But when you start adding on other things, like smoking, family members who have had pancreatic cancer, this permutation has significant increases. Patients with BRCA mutations could have risk-reduction surgery to lower their breast or ovarian cancer risk but, depending on their family history, they may also need to have endoscopic ultrasound exams and MRIs to look for pancreatic cancer.”
People who have their pancreatic cancer identified through screening do have a better chance of surviving this disease, but it’s still a rare cancer for which screening is limited and not widely discussed. “The question is, who are the best candidates for screening? For uncommon cancers, widespread screening programs like what we have for breast cancer or colorectal cancer are not helpful. The best candidates are individuals who have one or more risk factors that put them at the high-end of lifetime risk for developing pancreatic cancer, including people with premalignant tumors of the pancreas or people with a strong family history.”
High Risk Pancreatic Cancer Screening Risk Level Assessment Form
What can be done to decrease the risk of developing cancer?
The best way for someone to reduce their risk of developing cancer, regardless of family history, is to quit smoking, reduce alcohol consumption, work to maintain a healthy weight, and have an active lifestyle. This is the recommendation given by all four doctors: “There are general health benefits that go beyond cancer prevention for living a healthy lifestyle,” Dr. Fountzilas says. Having regular wellness checks with a primary care doctor is another good step to take, as it provides an opportunity to raise any concerns about changes in health or family history, and a primary care doctor will know when it’s time to consider early detection testing for cancer based on those factors.