Thanks to rapid advancements in technology, today we’re able to look deeper into the human body, detect cancer earlier, treat areas that once were inaccessible and perform surgery less invasively.
Roswell Park Comprehensive Cancer Center is out front in adopting and refining the newest, most promising technologies. Because we focus exclusively on cancer, we employ these tools to diagnose and treat large numbers of patients, which means our medical teams are highly experienced in their use. That’s why physicians from all over the world look to Roswell Park for training in robotic surgery and Gamma Knife radiosurgery. But we go beyond that: We’re global leaders in discovering new ways to use these and other procedures to help our patients live longer, healthier lives.
Thanks to the latest technology and the expertise of our clinicians, we’re armed with a powerful arsenal against cancer. Here are just six of the coolest technologies at Roswell Park.
Navigating ‘tiger country’ with a 3D map
The young woman’s thyroid cancer had returned, and the new tumor was “deep in her chest, hidden between the great vessels, in a location I could not access through the neck,” recalls Kimberly Wooten, MD, a head and neck surgeon at Roswell Park. So Dr. Wooten enlisted the help of a colleague, thoracic surgeon Anthony Picone, MD, PhD, MBA, FACP, FACS, formerly of Roswell Park, who would be able to reach the tumor through the chest.
But even with both of them working side by side, the situation posed major challenges. The carotid artery is just one of the major blood vessels that travel through that area of the body, so finding the safest route to the tumor was going to be complicated. It’s a situation Dr. Picone called “tiger country,” where nicking an artery or making an incision in the wrong place “could be a disaster.” Equally important, adds Dr. Wooten, she and Dr. Picone wanted to make sure they’d be able to locate and remove the entire tumor.
A bigger safety net
In most cases, CT scans provide all the information needed to plan an operation like this. But CT scans are cross-sectional (flat) images, and it's not easy to translate them into the 3D orientation the surgeons will encounter when they enter the three-dimensional world inside a patient's body. With CT scans, the surgeon has to visualize what the 2D images would look like if they were merged, explains Dr. Wooten, “and our brains don’t always work that way.”
Fortunately, Roswell Park surgeons can request a custom-made 3D “map” to provide a bigger safety net in regions of the body where the anatomy is highly complex.
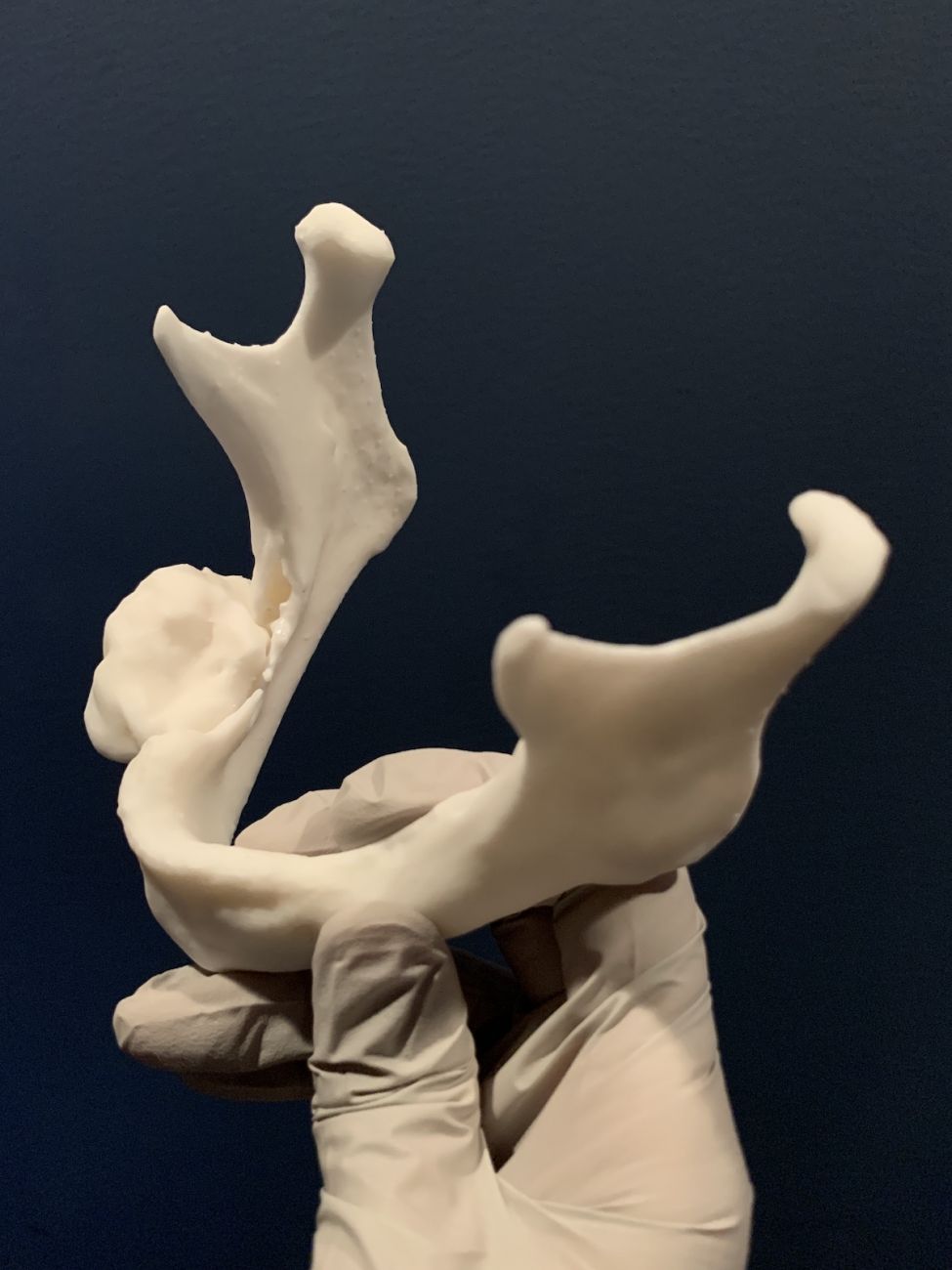
Dr. Picone held up a plastic model of the young woman’s tumor and the structures around it as they looked before surgery. Created from the patient's preoperative CT scan, the 3D printed model shows everything in intricate detail. “The model made it clear I was going to have to divide the breastbone to get safe exposure, that I would be able to get the tumor away from the arteries, and that I would be able to remove the tumor from the windpipe without too much trouble,” he said.
“And that turned out to be absolutely correct. There was no bleeding. Everything went perfectly well. This 3D reconstruction made it very safe.”
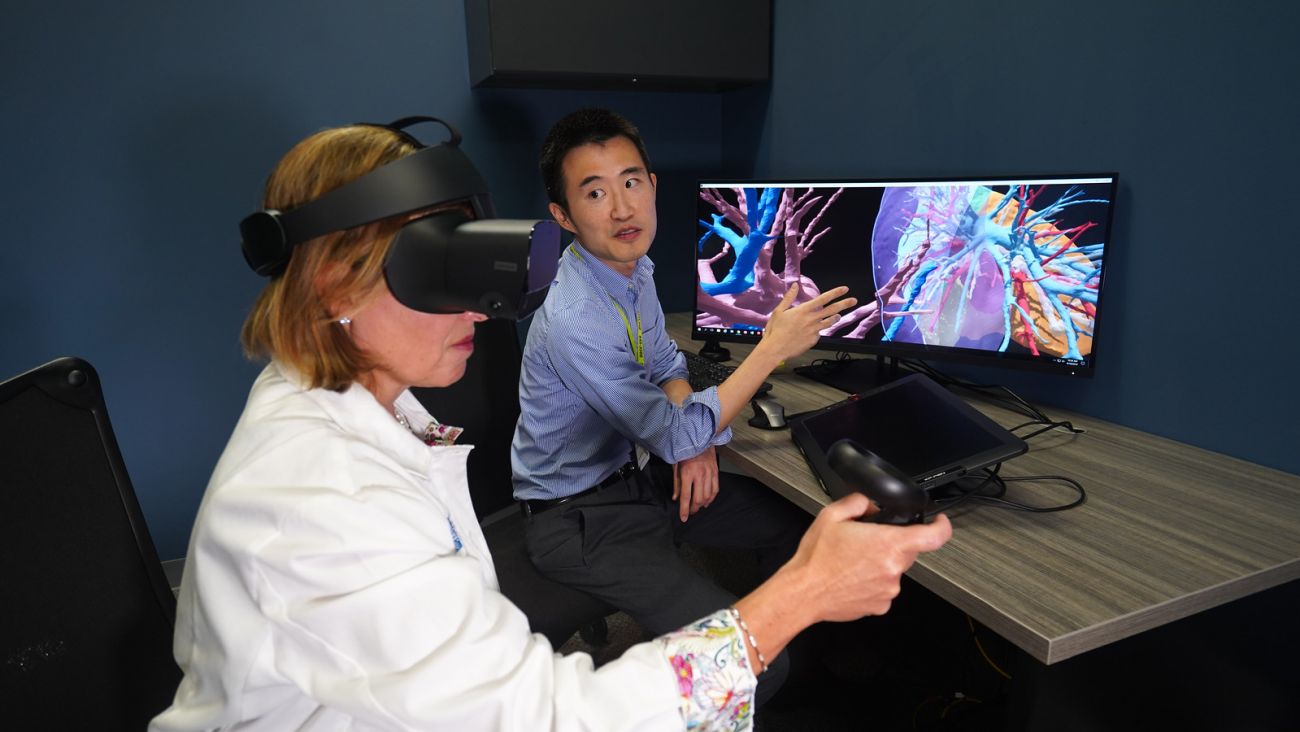
Reducing the extent of surgery
Diagnostic radiologist Larson Hsu, MD, created the plastic 3D model to help the surgeons “plan ahead for unexpected roadblocks.” Equipped with FDA-approved software, a tablet computer and a pen, he can transform a flat CT image of a tumor and the area around it into a computerized 3D image that can be rotated or flipped using a mouse or stylus. Taking it a step further, a surgeon can put on special goggles, view the tumor in virtual reality as if it’s floating in the air, and use a hand-held controller to rotate and enlarge it to explore the organs and other structures around the tumor.
Thanks to generous donations to the Roswell Park Alliance Foundation, Roswell Park now has 3D printers that enable Dr. Hsu to produce the type of plastic model Drs. Picone and Wooten used in their surgical planning. The printer can even add color, showing veins in blue and arteries in red, or print transparent areas. “You can print a transparent model of a prostate, for example,” explains Dr. Hsu. “The prostate will be almost completely clear, like crystal. The tumor will be inside it, which you can see in purple.”
Thoracic surgeon Todd Demmy, MD, FACS, finds 3D models helpful because “the arteries and veins in the lung are as variable as tree branches after a certain point, and you can’t really see them, because they’re covered with lung tissue. You have to know where they’re hiding, and the three-dimensional models give you that perspective.”
While 3D models are not necessary for most of his surgeries, Dr. Picone says they’re invaluable “when we have concerns about lung arteries and veins, or when tumors are located at very crucial points in the airway branching system. We can see things ahead of time that normally we can see only in surgery, so it gives us a heads-up of what we’re in for and how to strategize ahead of time.”
Dr. Hsu adds that studies have shown that using 3D printed anatomical models for reference can reduce how long the surgery takes, which in turn means better patient outcomes.
A benefit for lung-sparing surgery
The virtual models also can make it clear in advance whether the surgeon will be able to perform lung-sparing surgery, adds Dr. Picone. That is possible only if the tumor can be removed without injuring or dividing a major artery that spans both the upper and lower lobes of the lung. “In the old days, normally you would just take out the entire left lung, sacrificing both lobes. It’s not a big operation, but it’s tough on the patient. Nowadays we do lung-sparing surgery whenever we can.”
Recently Dr. Picone and Sai Yendamuri, MD, FACS, Chair of Thoracic Surgery, worked together on a patient who had a large tumor in the left lung. “It looked as if it involved the main pulmonary (lung) artery, so we used the virtual 3D reconstruction,” says Dr. Picone. “We saw exactly where the tumor was, and we knew exactly where we were going to have to cut.
“It was wonderful. The 3D reconstruction helped a lot in terms of figuring out whether we would be able to do it, and how to do it.”
Greater precision for head & neck prostheses
The same technology is emerging as an important resource for helping some patients with head and neck cancer. If a patient undergoes extensive cancer surgery — for example, having a nose or ear removed — prosthetic replacements can be created afterward to restore their appearance. With the traditional method, a mold is made from the patient’s face prior to surgery. The mold is then used to create the prosthesis, and the final shaping and coloration are finished by hand.
But Dr. Hsu can use the patient’s presurgery CT scan data to print a 3D model to match the patient's original facial structure. Made of biocompatible material designed to be in contact with the skin without causing allergic reactions, the model can be covered in skin-tone silicone so it's ready to go immediately after the cancer surgery.
“The possibilities are limitless”
Dr. Hsu says Roswell Park physicians are providing feedback as he continues to develop the system. For example, Dr. Wooten wonders if 3D imaging can be incorporated into robotic surgery simulators so surgeons in training can practice virtual surgery on a specific patient’s tumor before going into the OR to perform the actual operation. And Dr. Hsu foresees the possibility of projecting a 3D hologram of the tumor over the actual patient in the operating room, so surgeons will know exactly where the tumor is in relation to everything around it.
“It’s science fiction, but it’s not,” says Dr. Hsu. “It’s already happening; we have the technology. To me, the possibilities are limitless.”
Robotic bronchoscopy: flipping the odds for lung cancer patients
Most cases of lung cancer are detected when the disease is already in the advanced stages — one of the main reasons it’s the leading cause of cancer death. Discovering it in the early stages, when it can be removed surgically, “has far and away the best chance of cure,” says Nathaniel Ivanick, MD, (pictured) interventional pulmonologist in the Department of Thoracic Surgery.
That’s possible now at Roswell Park, where a new robotic bronchoscopy system will be “game-changing” for patients, according to Sai Yendamuri, MD, Chair of Thoracic Surgery, who spearheaded the move to acquire the system, called the Monarch. Catching lung cancer early “is both difficult and critical to survival,” he says.
Roswell Park is the first center in New York State and one of few in the nation equipped with the system, thanks to the generosity of donors to the Roswell Park Alliance Foundation. Combining the power of robotics, computer navigation and 3D imaging, the Monarch enables physicians to "travel" into the deepest recesses of the lungs to identify any suspicious areas and biopsy them. That means patients get the diagnosis they need without unnecessary surgery and begin treatment at a stage when it is more likely to be effective.
Using a controller similar to a gamepad used for video games, Dr. Ivanick maneuvers the bronchoscope into the patient’s airway. A high-resolution screen shows him the area where the suspicious lesion is located, while another screen provides a magnified 3D view of what the camera sees as it moves through the lungs and their passageways.
If he sees spots that might be cancerous, he can use the Monarch to remove tissue for biopsy. Until now, whenever CT scans showed suspicious spots that could not be reached for biopsy using conventional bronchoscopy, physicians had to either wait and see if the spots grew and started behaving like cancer — which carried the risk that the cancer would spread in the meantime — or perform surgery to do the biopsy, which could run the risk of lung collapse and other complications.
“I’ve had a number of cases where my chances of getting to a nodule with any other sort of platform would be really, really low,” says Dr. Ivanick. “And we’ve gotten it with the Monarch.”
Considering that about 77% of lung cancer cases are diagnosed in the late stages, Dr. Ivanick hopes this new technology will help flip the odds. If we could diagnose 77% of cases at stage 1, he says, “I think that would result in a lot of life-years saved and overall fewer complications from chemotherapy and other treatments used for more advanced stages of cancer.”
Benefits of robot-assisted surgery extended to patients with upper GI cancers
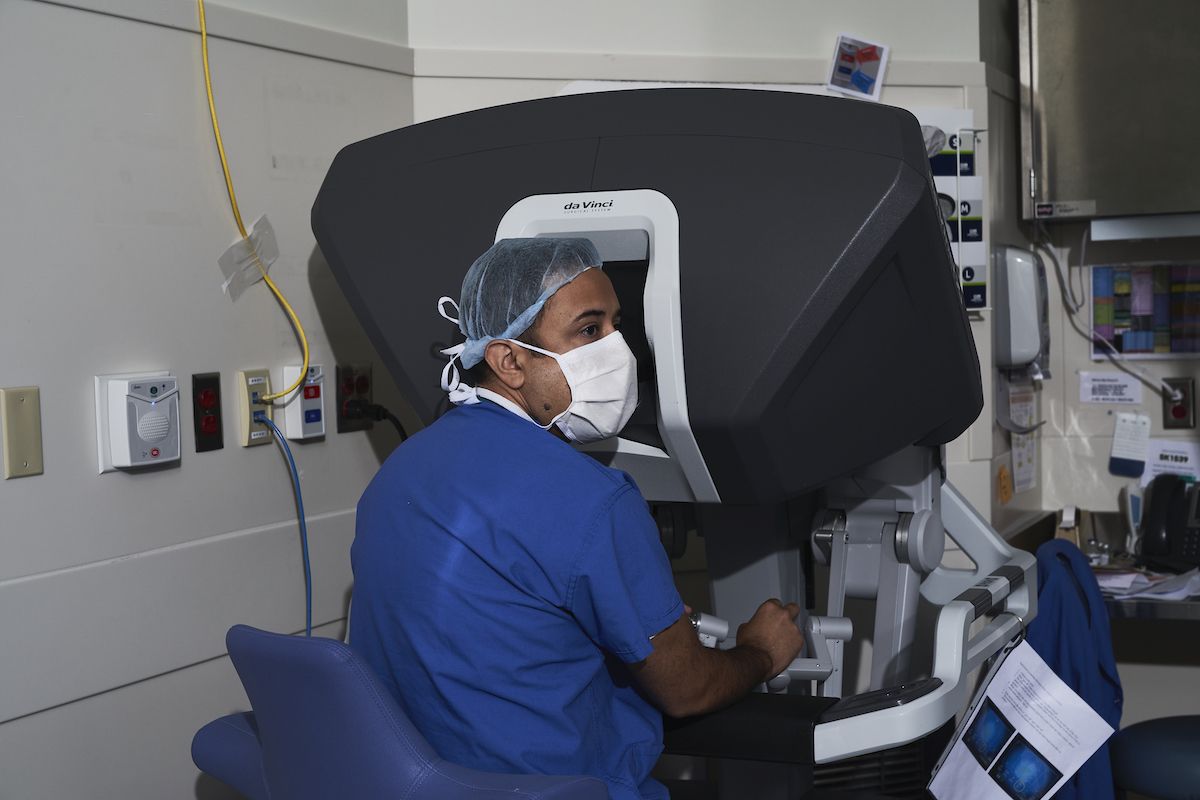
Introduced at Roswell Park in 2004, robot-assisted surgery (RAS) has led to shorter hospital stays, faster recovery and reduced pain for patients with many types of cancer: bladder, colorectal, gynecologic, head and neck, kidney and prostate. Thanks to the pioneering work of Moshim Kukar, MD, FACS, Department of Surgical Oncology, (pictured) and his Roswell Park team, now it’s also the standard of care for eligible Roswell Park patients with upper gastrointestinal (GI) cancers, including esophageal, stomach and pancreas.
Because operations for upper GI cancers are very complex and time-consuming, it has taken longer to develop robot-assisted techniques for that region of the body than for other disease sites. But Dr. Kukar and his Roswell Park colleagues are helping advance the procedure at both the regional and national levels.
What’s the advantage? RAS uses tiny incisions and is far less invasive compared with traditional “open” surgery, which requires larger incisions. At the same time, Roswell Park’s da Vinci® surgical robotic system equips the surgeon with a 3D view of the operating field and instruments that can swivel in tight spaces. “It is an amazing tool and extremely precise,” says Dr. Kukar.
There’s a striking difference in the recovery experience of patients with esophageal cancer who undergo traditional open esophagectomy (removal of the esophagus) versus those treated with RAS, Dr. Kukar adds. Open-surgery patients “sometimes spend two or three days in the ICU due to significant pain and other issues. With the robotic approach, our patients are up and walking around the day after surgery. They don’t go to the ICU routinely; they spend just one day in a ‘step-down unit’ before moving to a regular floor.”
Esophagectomies are highly complex operations, he explains, because they involve “two different body cavities — the chest and the abdomen.” The surgeries last between seven and eight hours on average, and that can be especially grueling during a traditional open surgery, where the surgeon stands beside the operating table the entire time. There’s less fatigue during a RAS procedure, with the surgeon manipulating the surgical instruments while sitting at a console.
Most important, Dr. Kukar’s research comparing traditional laparoscopic and robotic surgical techniques for esophagectomy has shown that RAS is associated with less blood loss, a shorter hospital stay, fewer complications and the ability to remove more lymph nodes.
Challenging operations
Because training in robotic surgery involves a steep learning curve, the surgeon’s skill level depends largely on the number of surgeries performed, says Dr. Kukar. When someone with less experience sits at the console, a RAS esophagectomy that normally takes seven hours can go on for 10, 12 or even 14 hours, pushing the limits of safety. “That’s why it’s critically important to have this surgery done at a high-volume center, because these are challenging operations to begin with. There’s not a lot of room for error.”
Nationally, the risk of dying from the operation within 30 days is close to 5-7%, although it’s lower in hospitals that perform a high number of the procedures. In well over 300 patients evaluated at Roswell Park, the 30-day mortality rate was 0%.
A world leader in robot-assisted surgery, Roswell Park has treated more than 6,600 patients with this technique since 2004 and trained hundreds of surgeons from more than 14 countries around the world. Roswell Park surgeons have performed more than 100 RAS esophagectomies — one of the largest volumes at a U.S. center — and Roswell is the only center in Western New York offering robot-assisted Whipple procedure for pancreatic cancer.
With the rapid evolution of robotic surgical systems and five new surgical robots expected to enter the market by 2025, Dr. Kukar says that in addition to treating complex cancers using the technology that’s currently available, he and his team are also looking down the road, evaluating technology that’s still in the pipeline, “so we can take a leadership role in developing newer technology and bringing it to our patients.”
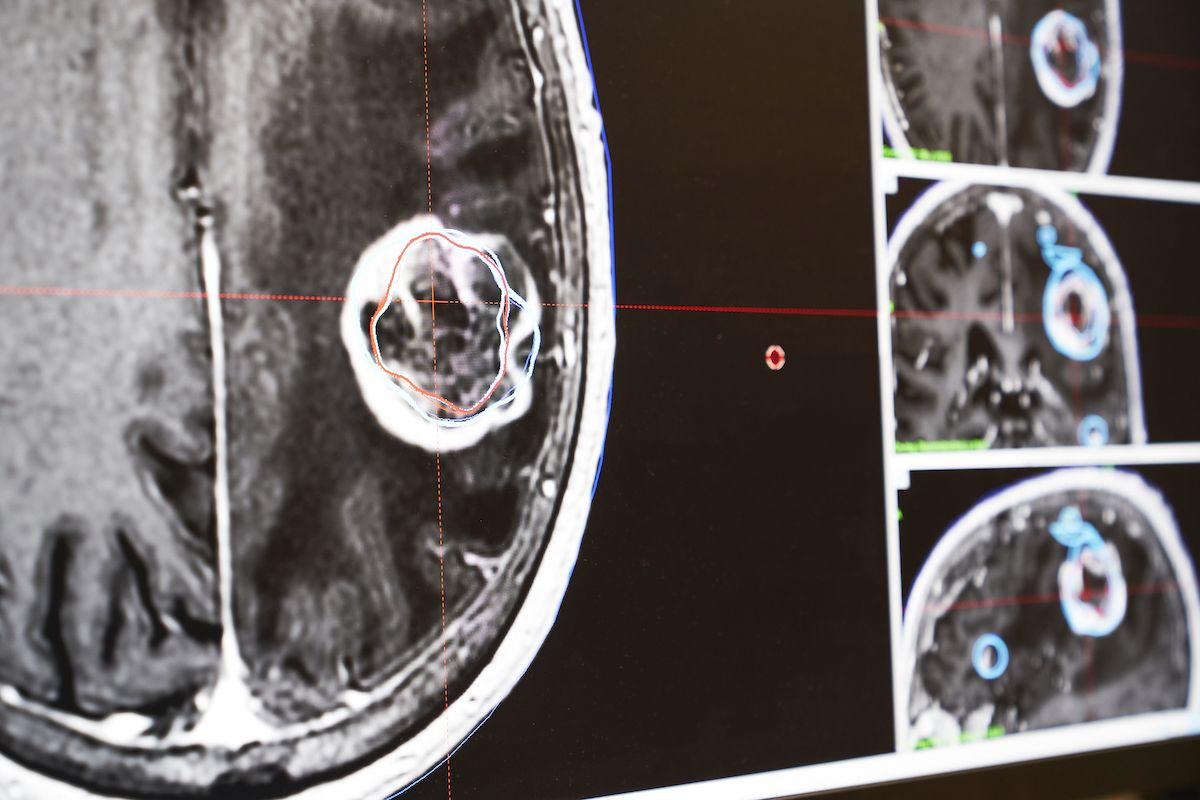
A revolutionary way to identify metastatic brain tumors so treatment can begin earlier
Two revolutionary new software packages are taking Gamma Knife radiosurgery to a whole new level at Roswell Park, bringing world-class treatment to patients with specific types of brain tumors and disorders.
Roswell Park is the only center in Western New York equipped with the Gamma Knife Icon, a radiosurgery system that eliminates the need for a craniotomy (opening the skull) to remove specific types of brain and pituitary tumors and to treat such conditions as acoustic neuroma and essential tremor. Unlike conventional brain surgery, Gamma Knife radiosurgery doesn’t involve a scalpel. Rather, it zaps brain lesions with 192 intersecting beams of gamma radiation to destroy tumors and other abnormalities without harming healthy tissue. Patients are awake during treatment and go home immediately afterward.
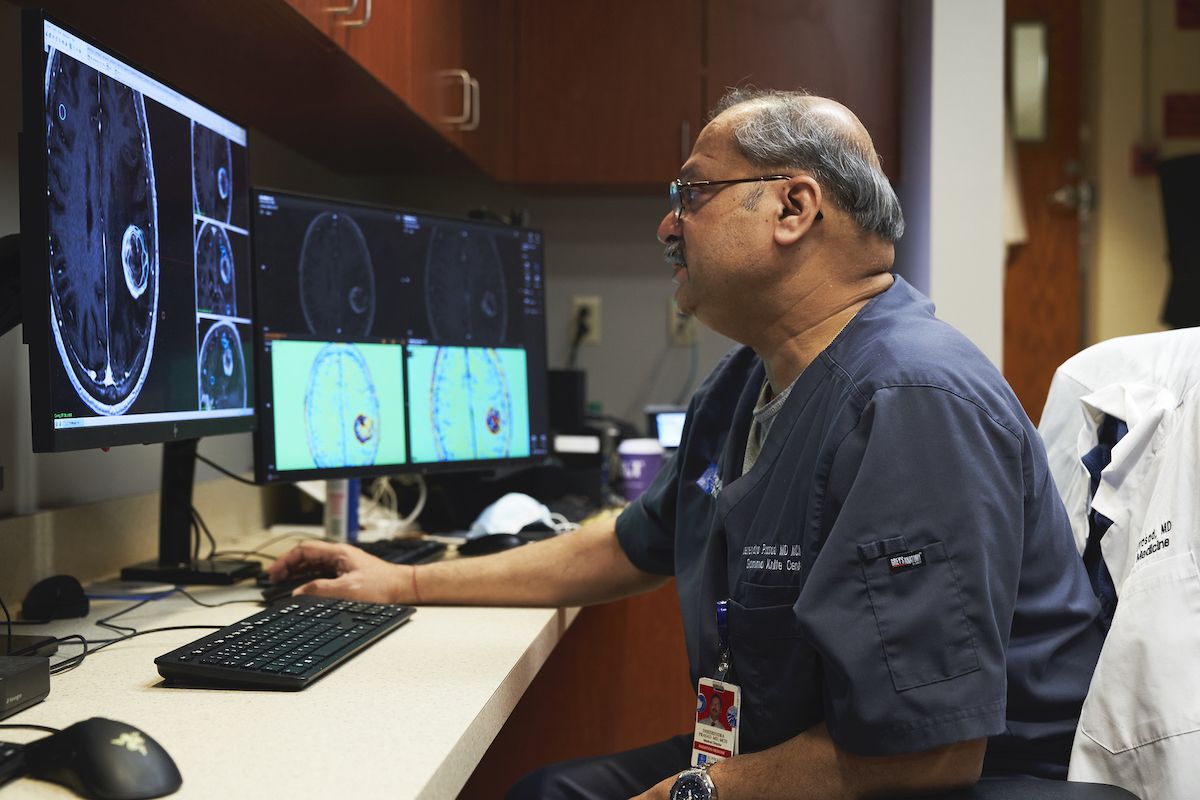
Roswell Park was the first center in the U.S. to acquire one of the new software packages, called Lightning, which transforms the Gamma Knife Icon into the most advanced radiosurgery system in the world. That’s due to the stature of Dheerendra Prasad, MD, MCh, FACRO, Director of Roswell Park’s Gamma Knife Center, a leader in refining the Gamma Knife system and an expert who trains physicians from around the world how to use it. “We were one of few centers that were part of a collaborative agreement for beta-testing the software, providing feedback and doing research,” says Dr. Prasad.
Lightning gives physicians the power to:
- Develop treatment plans much faster and more efficiently while improving the quality of the plans. “We can generate several versions of a treatment plan and compare them and pick the one that makes the most sense for the patient, and we can do that pretty quickly,” says Dr. Prasad.
- Reduce treatment time, making the experience more patient-friendly. “They appreciate the fact that they can get on and off the table quicker,” he says.
Using a second new software package, Brainlab Elements®, Roswell Park’s Gamma Knife and Radiology teams have pioneered a new method of identifying metastatic brain tumors in patients who previously received radiation treatment to the brain, so treatment can begin earlier with the aim of better controlling the cancer. “No one else has done that anywhere in the world,” notes Dr. Prasad.
In the past, if imaging after radiosurgery treatment showed suspicious areas in the brain, it would be impossible to tell whether the spots were tumors that had recurred or simply the aftereffects of radiation. The only way to find out was to wait a few months to see whether they grew — but waiting could allow the cancer to progress.
Contrast clearance analysis, a feature of Brainlab Elements, makes it possible to quickly tell the difference through color-coding, and Roswell Park was first to apply the idea to metastatic tumors. “Now we can identify them earlier,” says Dr. Prasad. “If a patient comes in for a follow-up and we find a new spot and have time that day, they get treated the same day” — getting ahead of the tumor as fast as possible.
“It can be as little as zero days from diagnosis of a metastatic brain tumor to treatment,” he adds. “Ninety-five percent of our patients are treated within 10 days.”
Dr. Prasad says this new capability “improves the efficiency of the treatment. Of course, it will take time to demonstrate clinically that it improves outcomes, but it’s the direction we want to go.
“We like to stay at the cutting edge and make sure we have what it takes to be ready for the next step. This software positions us to be ready for other next-generation changes in the Gamma Knife and radiosurgery world.”
For example, with Lightning in place, Roswell Park is ready for the introduction of the latest carbon-fiber head frames that will be available in the near future, he says. The frames are used to keep the patient’s head steady during treatment. “They will allow us to see tumors in a much more precise manner, which will allow us to expand the conditions we can treat,” he explains. “When they get the frames to us, we can start using them with the Gamma Knife in the clinic the next day.
“Patients in Western New York who get treated at Roswell Park with the Gamma Knife are getting the latest and best treatment. They can go far and wide and not do better.”
Roswell Park’s Gamma Knife is the busiest single system of its kind in the world and was used to deliver over 700 treatments in 2020 alone.
For inoperable cancers, a choice of ablation options
Imagine finding out that surgery is the best treatment option for your cancer, but you’re not eligible. That can happen if other medical conditions mean an operation is too risky for you, or if previous surgeries would make another surgery difficult or impossible.
For many patients at Roswell Park, ablation provides a noninvasive alternative, says Michael Petroziello, MD, Department of Diagnostic Radiology (pictured). It’s a way of killing tumors with extreme heat, extreme cold or electrical currents.
“There are no incisions,” he explains. Guided by CT scan and ultrasound imaging, he and his colleagues insert a needle into the tumor to deliver the cancer-killing energy. Patients receive an intermediate level of anesthesia, and in most cases go home the same day.
Roswell Park provides:
- Microwave ablation, which involves very high heat. This is used most often for small tumors in the liver and lung.
- Cryoablation, which involves extreme cold. This is used mostly for tumors in the kidney and for musculoskeletal tumors. “The musculoskeletal tumors we see tend to be a little bigger,” says Dr. Petroziello, “and cryoablation gives us the option of covering a much bigger area than microwave ablation could.”
“We can tailor the ablation technology to the type of tumor they have,” says Dr. Petroziello.
He adds that most patients tolerate the procedure very well but might experience mild pain afterward. “They may have mild discomfort for two or three days afterward that can be relieved with over-the-counter medication. Some patients also experience mild nausea right after the procedure, but it’s usually gone by the time they go home.”
As with other medical procedures for cancer, Dr. Petroziello advises that patients undergoing ablation “should go to a center where the team performs a lot of these. At Roswell Park, we see a lot of these patients and perform several of these procedures a week.
“It’s not just that we have all the technology available — it’s also that we’re experienced enough to know which technology to apply to a specific patient to achieve the best outcomes,” he says. “That puts Roswell Park a step ahead in upstate New York.”
Super vision: a powerful new tool for neuro and head & neck surgeries
Removing a brain tumor poses special challenges. The tumor can look very much like healthy brain tissue — where does one end and the other begin? — and it may also be close to “complex anatomy of other structures, such as nerves and blood vessels,” says Roswell Park neurosurgeon Lindsay Lipinski, MD, FAANS.
The Olympus ORBEYE, a surgical visualization tool, dramatically enhances the view of the surgical field for Roswell Park’s Neurosurgery team, providing a magnified, 3D image that gives them the best chance of removing the tumor completely with the highest level of safety.
Before the arrival of the ORBEYE, the neurosurgeon and assistant peered through lenses on opposite sides of a bulky microscope suspended over the patient. The microscope restricted their movements and gave each of them a slightly different perspective of the surgical site. Now, wearing special high-quality 3D glasses, both of them look up at a large screen to see a magnified, 3D view of the patient’s brain that helps guide them along the safest path. ORBEYE’s exceptional lighting sharpens every detail.
Not only do both surgeons see exactly the same view of the brain, but other members of the surgical team can see it, too, “so it allows the entire team to know what’s happening in real time during the surgery and be better prepared” for what will happen next, explains Dr. Lipinski.
The technology will become even more powerful with the FDA’s expected approval of the use of the drug 5-ALA with the ORBEYE, according to Robert Fenstermaker, MD, Chair of the Department of Neurosurgery and Director of the Neuro-Oncology Program. Given to the patient before neurosurgery, the drug settles in tumor cells and “makes them glow bright pink under blue light,” says Dr. Fenstermaker. “The benefit is that it enhances our ability to distinguish small bits of tumor from normal tissue. We plan to use it once it is approved for use with ORBEYE.”
The benefits of the ORBEYE system extend to reconstructive surgery as well. Ryan McSpadden, MD, a head & neck and plastic & reconstructive surgeon at Roswell Park (pictured on the left in the operating room with Hisham Hatoum, MD), uses it for reconstructive surgery of the head and neck. He says the system “allows for a magnified view of blood vessels and nerves so we can perform microsurgery to reconnect those structures when performing tissue transplants.”
Roswell Park is the only center in Western New York equipped with the ORBEYE — a technology that has transformed surgical treatment for many of our patients.