Two Roswell Park clinical trials aim to find out
Patients with esophageal cancer typically face a poor prognosis, with a five-year relative survival of only 21%. But researchers at Roswell Park Comprehensive Cancer Center have launched two clinical trials in the hope that a commonly prescribed blood pressure drug can change that outcome.
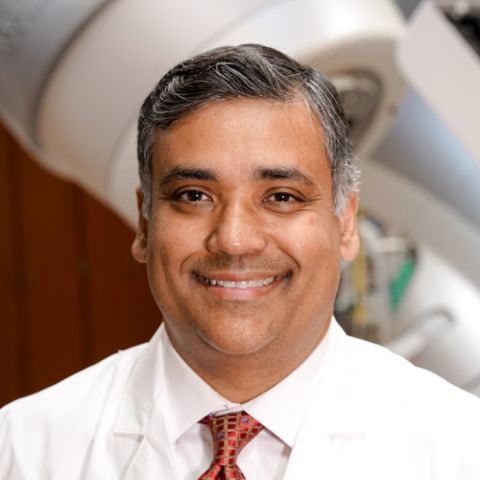
The poor survival rate is due largely to the fact that most patients with esophageal cancer have advanced disease at the time of diagnosis, explains Sarbajit Mukherjee, MD, MS, gastrointestinal medical oncologist in the Department of Medicine, Co-Leader of the GI Translational Research Group at Roswell Park and principal investigator (PI) of one of the studies. “Most of the time it has already spread to adjacent lymph nodes or distant organs, and it is resistant to treatment.”
Patients with metastatic disease that has spread to other parts of the body, or those whose disease cannot be treated surgically, are usually treated with a combination of an immunotherapy called a checkpoint inhibitor — such as pembrolizumab (brand name Keytruda) or nivolumab (brand name Opdivo) — along with chemotherapy, yet survival remains poor. “For the most part, these cancers are not very responsive to immunotherapy,” explains Dr. Mukherjee. “They respond initially to chemotherapy, but the cancer finds a way to beat the chemotherapy, and it becomes progressive.”
Dr. Mukherjee and his Roswell Park colleagues want to find out whether a beta blocker called propranolol (brand name Inderal) can improve the efficacy of checkpoint inhibitors. Approved by the FDA in 1968, propranolol is commonly used to treat high blood pressure.
Stress suppresses the immune system
The strategy for the two clinical trials first took shape in the lab of Elizabeth Repasky, PhD, Vice Chair of Immunology and Co-Leader of the Cancer Stress Biology Program at Roswell Park. Her team discovered in preclinical research that when the body is under chronic stress, activated nerves produce a hormone called norepinephrine, which weakens the immune system’s ability to fight cancer. Propranolol blocks the action of norepinephrine.
The discovery provides part of the answer to an age-old question, says Dr. Repasky: “If two patients are diagnosed with the same type and stage of cancer, why is it that sometimes one patient will be cured while the other will later die of the disease?” She says there’s evidence that patients who experience a higher level of stress have a higher risk that their tumors will grow and metastasize faster.
“Earlier Roswell Park clinical trials for other types of cancer have demonstrated that beta blocker drugs like propranolol relieve that stress and allow anti-tumor immune cells to become much stronger, which gives immunotherapies — and in particular, checkpoint inhibitors like pembrolizumab — a much better chance to work,” she adds.
For example, a phase 1 clinical trial led by Shipra Gandhi, MD, Department of Medicine at Roswell Park, combined propranolol with pembrolizumab to treat patients with metastatic melanoma, resulting in an unprecedented response rate of 78% (the percent of patients whose tumors shrank or vanished after therapy).
Anurag Singh, MD, Director of Radiation Research in the Department of Radiation Medicine and Co-Leader of the Cancer Stress Biology Program, says he and his colleagues found evidence of propranolol’s potential for treating esophageal cancer in a database of information about patients who were treated for the disease with chemotherapy and radiation (chemoradiation) at Roswell Park. They found that those who were taking beta blockers at the time of treatment fared better. “The association was quite positive,” he says.
Both of the current clinical trials are enrolling patients with adenocarcinomas of the esophagus or gastroesophageal junction, the area where the esophagus connects to the stomach. Adenocarcinomas are cancers that grow in the glandular tissue of specific organs, such as the esophagus and stomach, and produce fluids such as mucus and digestive fluids.
“Significant opportunity to potentially change the standard of care”
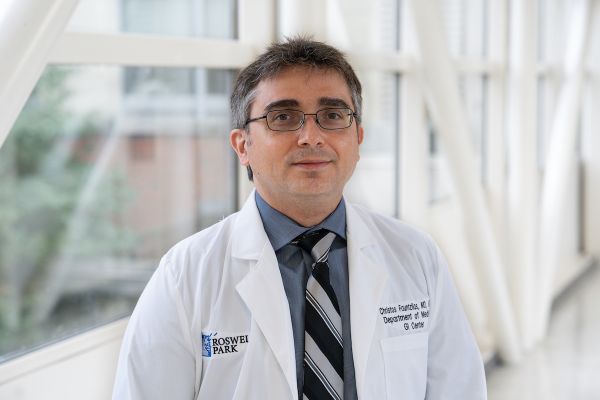
“Roswell Park is at the forefront of research on gastroesophageal cancer, and these two studies incorporating beta blockers are aiming to improve the efficacy of chemotherapy, immunotherapy and radiation in those patients,” says Christos Fountzilas, MD, FACP, Co-Leader of the Gastrointestinal Clinical Disease Team and Associate Director for Solid Tumors with the Early Phase Clinical Trials Program at Roswell Park. Dr. Fountzilas was co-author of an article in the journal Lancet showing that adding pembrolizumab to chemotherapy improves overall survival significantly in patients with gastroesophageal cancer — a finding that led the Food & Drug Administration to approve the use of pembrolizumab for treating the disease.
Never miss another Cancer Talk blog!
Sign up to receive our weekly Cancer Talk e-newsletter.
Sign up!Dr. Mukherjee’s study, "A phase 2 trial of chemotherapy, pembrolizumab and propranolol in advanced esophageal/gastroesophageal junction adenocarcinoma patients” (NCT05651594), will enroll 40 patients. They will receive the standard-of-care combination chemotherapy along with pembrolizumab and propranolol. “We are very encouraged by our preclinical data and our initial phase 1 clinical patient data,” says Dr. Mukherjee.
Dr. Singh will serve as PI of the second study, a randomized clinical trial that will evaluate the effects of propranolol when it is combined with chemoradiation. The study, “Propranolol with Standard Chemoradiation for Esophageal Adenocarcinoma” (NCT04682158), will enroll 60 patients. All patients will receive standard-of-care chemoradiation prior to surgery, and some will also be chosen randomly to receive propranolol. Patients who were already on a beta blocker prior to the study will receive chemoradiation alone.
“We haven’t made any significant advances against esophageal cancer in many, many years,” says Dr. Singh. “These two clinical trials represent a significant opportunity to potentially change the standard of care for esophageal cancer.”