New combinations of therapies are offering hope to patients with esophageal cancer.
Typically, esophageal cancer — either squamous cell esophageal cancer or adenocarcinoma — is treated with a combination of chemotherapy, radiation and surgery to remove the tumor from the esophagus. The patient’s tumor will be examined to see whether there is residual cancer left in the sample specimen; if there is, patients have a higher risk of a relapse or recurrence.
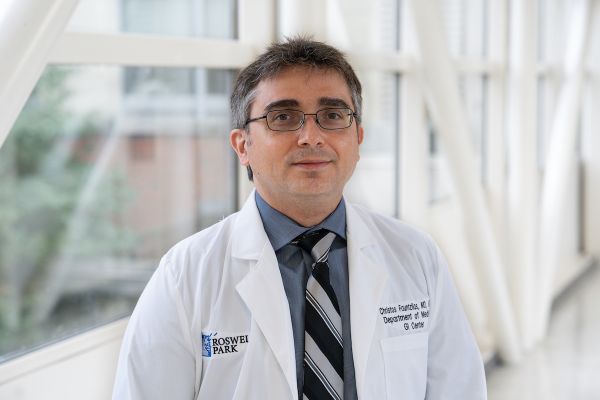
"Most patients do not have what is called a complete pathological response to their initial treatment", says Sarbajit Mukherjee, MD, MS, a medical oncologist specializing in gastrointestinal cancers at Roswell Park Comprehensive Cancer Center. “Those patients who have some residual cancer in their surgical specimen typically have a very high chance of recurrence and the cancer tends to come back quickly. We didn’t know what to do for those patients,” who would then be kept under observation.
In the United States, adenocarcinomas, which begin in the gland cells in the lower third of the esophagus, are the most common type of esophageal cancer. Risk factors include a history of acid reflux or gastroesophageal reflux disease (GERD). Worldwide, however, squamous cell carcinoma, which begins in the squamous cells of the esophageal lining, is more common. Risk factors include a history of smoking, alcohol consumption and poor oral hygiene. New immunotherapies present new options for both types of esophageal cancer.
Three studies, three new combination treatments
If the patient’s cancer didn’t respond to chemotherapy and radiation, options were limited other than a wait-and-see approach. But new research has found that the introduction of an immunotherapy medication, nivolumab (commercial name Opdivo), can dramatically improve their response.
“What the researchers did was look at patients who didn’t have a complete pathological response to treatment and randomized them so some received nivolumab. The patients who did receive nivolumab had a nearly double disease-free survival and their chance of having the disease come back was significantly less. Based on that, this drug was approved for those patients. It’s totally practice-changing,” Dr. Mukherjee says.
But that’s not all: Other clinical trials looked at the use of immune checkpoint inhibitors (like nivolumab), a class of drugs that block proteins on cancer cells and help the body’s immune system “see” the cancer and attack it more aggressively. For some metastatic esophageal cancer patients, receiving an immune checkpoint inhibitor in addition to chemotherapy found that these patients responded well to treatment, without the adverse effects typically associated with chemotherapy, and it improved their survival rates, Dr. Mukherjee says. Two different studies found similar results for both nivolumab and pembrolizumab (commercial name Keytruda), with pembrolizumab approved for use in treating squamous cell esophageal cancer and both drugs approved for use in combination with chemotherapy for adenocarcinoma.
In a third study, patients who had gastroesophageal junction (where the esophagus joins the stomach) cancer and carry the HER-2 gene overexpression — the same genetic change associated with aggressive types of breast cancer — were given the targeted therapy drug trastuzumab (commercial name Herceptin) in addition to chemotherapy and pembrolizumab as treatment for their advanced cancer. “This study showed that when you combine pembrolizumab with chemotherapy and trastuzumab, those patients did really well,” Dr. Mukherjee says. “Almost everybody had some sort of stability or disease control and a significant portion of patients had disease response. The overall response rate was 75%, but if you look at whether a patient had any decrease at all, 97% of the patients had some decrease. That is quite significant. This study will mature, and we will see what the data looks like, but this is very promising and practice-changing.”
All three treatment options are currently available for patients being treated for esophageal cancer at Roswell Park, he adds.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!The importance of clinical trials for esophageal cancer
Esophageal cancer is a rare disease in the U.S., with less than 20,000 cases diagnosed every year and, sadly, it does not have a high long-term survival rate. These studies, and these new combination therapies, are encouraging that patients given an esophageal cancer diagnosis can have better odds.
“We know immunotherapy works very well,” Dr. Mukherjee says. “Some patients can go on and live for years with a stage four disease, which was unprecedented before immunotherapy became available. Not everyone will respond to immunotherapy. We are still trying to figure out who will respond best to it, and there are now some biomarkers we are looking into. We’re looking at a patient’s PDL-1 status and finding that the higher their score, the more likely a patient will respond to immunotherapy. It’s a nice correlation but it’s not 100%.”
The next front in this research is to determine how to make immunotherapies work even better. This is where Roswell Park researchers like Dr. Mukherjee and his team are focusing and why he encourages his patients and their families to consider enrolling in clinical trials for new treatments.
“You can get standard treatment anywhere, but here at Roswell Park, we are always trying to move the bar so we can have more patients benefit from immunotherapy,” he says. “All this progress was made only recently and it’s only possible because patients and their families graciously agreed to participate in these studies.”