Roswell Park researchers focus on making cellular therapies safer, more effective, available to more patients
The Innovation Engine series highlights high-impact Roswell Park science that advances the priorities of the National Cancer Plan — a roadmap for working together to end cancer as we know it. The work outlined in this post supports Goal #3: Develop Effective Treatments and Goal #5: Deliver Optimal Care.
What if a patient’s own immune system could cure cancer? The idea has captivated researchers for more than a century, but only recently have we begun to realize the power of “living drugs” — the very cells coursing through a patient’s body. With cutting-edge research and the expansion of its GMP Engineering & Cell Manufacturing Facility, Roswell Park Comprehensive Cancer Center is making rapid advances toward the introduction of new cellular therapies for blood cancers and all types of solid tumors.
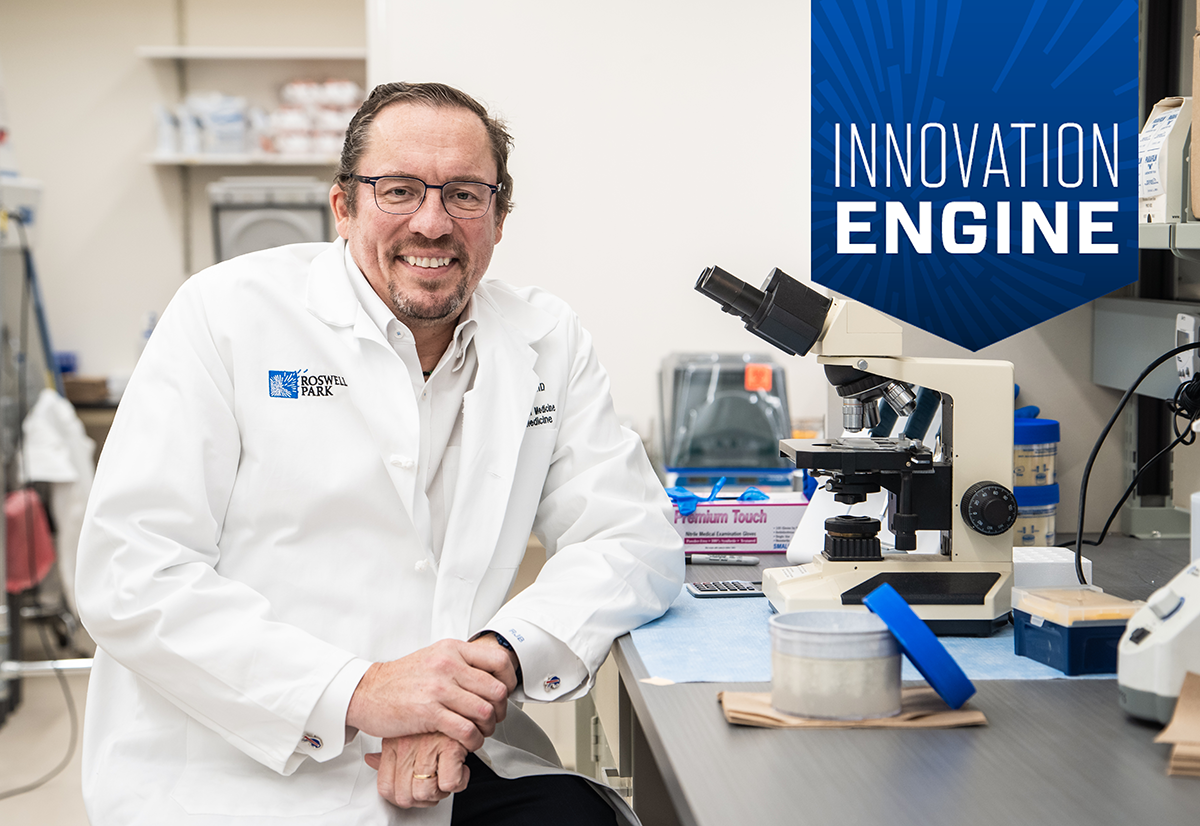
“We’re moving these therapies from the laboratory to the clinic,” says Renier Brentjens, MD, PhD, Deputy Director and the Katherine Anne Gioia Endowed Chair in Cancer Medicine at Roswell Park. “We anticipate that at some point in the foreseeable future, we will have a clinical trial available for any person with any type of cancer that has relapsed or is resistant to treatment.”
Cellular therapy has been around for decades — blood cancers have been treated successfully with stem cell transplants since the 1950s — but today a new frontier has opened, thanks to a better understanding of the power of special white blood cells called T lymphocytes, or T cells. Part of the immune system, they patrol our bodies and defend us against germs. They can also destroy cancer cells, but because cancer can adapt and remain “hidden” or evade treatment, T cells can’t always do that job effectively.
That’s where “re-engineering” comes in. One especially promising type of cellular therapy, chimeric antigen receptor (CAR) T-cell therapy, involves collecting a patient’s T cells, modifying them in the laboratory by adding a gene that will help them find and destroy the patient’s specific type of cancer, multiplying them into an army of millions and then returning them to the patient.
“Cellular therapies have shown a great deal of efficacy in patients who had no treatment options before this,” says Dr. Brentjens. “About 40% of patients achieve long-term remission or cure.”
Recognized as a pioneer in the field of cellular therapy, before coming to Roswell Park Dr. Brentjens launched the first laboratory studies showing that a patient’s T cells could be re-engineered to zero in on CD19, a protein on the surface of cells in some blood cancers — also called “liquid tumors” — and destroy them. He transferred those findings to the clinic to treat patients with CD19-positive leukemias that had returned after treatment.
The Roswell Difference
Pioneering innovation like this is part of what makes Roswell Park an "Exceptional" comprehensive cancer center, designated by the National Cancer Institute.
Extending the benefits to patients with solid tumors
Since 2017 the FDA has approved six CAR T-cell therapies for blood cancers, such as leukemia, lymphoma and multiple myeloma, but to this day there are no CAR T therapies approved to treat solid-tumor cancers. Now Dr. Brentjens and his Roswell Park colleagues are focused on extending the benefits of cellular therapies to patients with many other types of solid tumors. “Can this work with more common cancers — colon cancer, ovarian cancer, prostate cancer?” he asks.
The main challenge: solid tumors have a stronger defense system. They’re protected by the tumor microenvironment, a protective cocoon of blood vessels, immune cells that feed the tumor instead of fighting it, and fibroblasts — cells that prevent cancer-killing immune cells from entering the tumor or even being able to recognize it.
Information generated by a new clinical trial at Roswell Park may point the way forward. Led by principal investigator Francisco Hernandez-Ilizaliturri, MD, Director of Lymphoma Research and Director of the Lymphoma Translational Research Lab, the study will evaluate a new “armored CAR” T-cell therapy for specific lymphomas or chronic lymphocytic leukemia that resists treatment or has returned after treatment.
Patients’ T cells are re-engineered in two different ways — first with the addition of a CAR to help them seek and kill CD19-positive cancer cells, and then with a gene that “armors” them by stimulating them to produce a protein called IL-12, which may improve the immune system’s ability to fight the cancer. Investigators believe the same strategy could help overcome the protective barrier of the tumor microenvironment to combat solid tumors more effectively.
The clinical trial marks the first time patients’ T cells will be manufactured in Roswell Park’s Engineering & Cell Manufacturing Facility, which is certified as meeting the FDA’s stringent standards for producing pharmaceuticals. With the conclusion of a major expansion project next year, the facility will be the largest of its kind in New York State and the largest of any academic institution in the nation.
“We will not only be able to develop and run clinical trials for therapies generated in our own labs at Roswell Park, but we’ll have the opportunity to work with biotechnology companies to run some of their promising cell therapy clinical trials,” says Dr. Brentjens. “What that means for our patients is that as we support more and more of those trials, we’ll be able to offer clinical trials for more and more solid tumor cancers.”
Roswell Park investigators expect additional cellular therapy clinical trials to open in the years ahead, including:
- An “armored CAR” therapy designed to target the antigen DLL3, found on the surface of cells in small-cell lung cancer.
- A CAR T-cell therapy targeting the LRRC15 protein in pediatric and adult sarcomas.
- A CAR T-cell therapy targeting the CD83 protein, found in acute myeloid leukemia and Hodgkin lymphoma.
Preventing graft-versus-host disease in stem cell transplant patients
Roswell Park researchers also are making monumental strides toward improving the safety of another form of cell therapy in wide use over the last four decades: stem cell transplants. Patients who receive cells from a healthy donor — a procedure called an allogeneic transplant — can develop a serious and sometimes fatal side effect called graft-versus-host disease (GVHD), which occurs when the donor’s T cells perceive the patient’s cells as foreign and attack them. A study led by Shernan Holtan, MD, Chief of Blood and Marrow Transplantation, reported that a cyclophosphamide-based drug combination reduced patients’ risk of both acute and chronic GVHD by 50%. Published in the New England Journal of Medicine, the study is likely to change the standard treatment for these patients.
What’s next? Stay tuned. As Dr. Brentjens says, “There’s more to come.”