What if doctors were able to identify, with a simple blood test, when a patient’s cancer was starting to make a return? Or that a person’s disease was so well treated it would not return?
That’s the futuristic goal of the Immune Monitoring Resource and its director, Peter Maslak, MD, a new addition to the team at Roswell Park Comprehensive Cancer Center with more than 30 years’ experience in hematology, pathology and immunology. The program is fully funded by donor support through the Roswell Park Alliance Foundation.
“Immune monitoring is a surrogate for response to treatment,” explains Dr. Maslak, who also serves as Vice Chair for Clinical Affairs and is the Director of the Flow Cytometry Shared Resource at Roswell Park. “It’s an evolving field, because it’s not like giving a patient a test to measure the level of potassium in their blood after they receive a potassium supplement.”
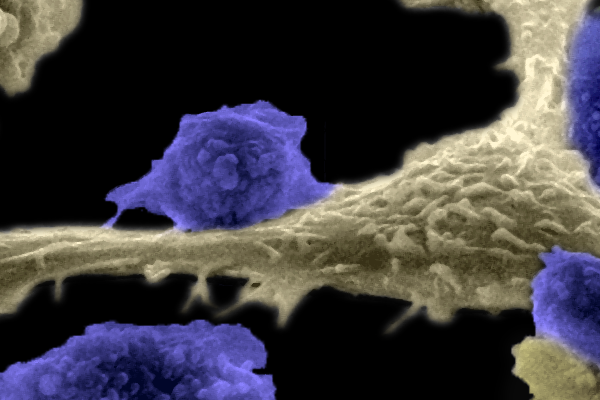
With immune monitoring, blood tests are used to measure the number of immune cells – lymphocytes – circulating in the patient’s body. For patients who have had a bone marrow transplant, for example, looking for the presence, and amount, of lymphocytes in their blood can be an early indication of whether they’re having a positive response to treatment and a successful transplant.
For patients who have received immunotherapy, including CART-cell therapies — in which the patient’s own cells are removed, modified to respond to and attack cancer cells and then reinfused to the body — immune monitoring can evaluate the effectiveness of those modified T cells in fighting the cancer.
“We’re developing better tests to actually look at the efficacy of the intervention we’ve done for you in terms of the cellular therapy, what some people call a living drug,” Dr. Maslak says. “We’re measuring not only the activity of the living drug we’re giving you, but also its effect on your body and the effect on other factors like your genetic make-up that may determine your response to therapy.”
A more accurate view of treatment response
By measuring the response to therapy, doctors can better anticipate whether and when someone might relapse and gather information that could help determine why one patient is responds better to treatment than others.
“If someone’s starting to have a relapse, being able to tell that earlier would provide a way for us to intervene earlier,” Dr. Maslak says. “For certain types of leukemia, we have really fancy molecular tests. If we can tell the person that there’s molecular evidence of a relapse, intervening early could work better than waiting for them to have a full relapse.”
“The idea is to predict how well treatment is working and, if there’s an issue, such as a dip in some biomarker that we’re using, we can make the response better,” he says.
Immune monitoring is done by piggybacking onto the routine blood tests most cancer patients already are used to undergoing, such as a complete blood count (CBC) in which red and white blood cells and platelets are counted. “After the patient has received their intervention or infusion, their blood would be tested for the population of different cells pertaining to their cancer,” Dr. Maslak says.
Never miss another Cancer Talk blog!
Sign up to receive our weekly Cancer Talk e-newsletter.
Sign up!Developing more powerful tools for the future
Roswell Park offers immune response monitoring to people with hematologic cancers. However, there is great hope that, as the technology and testing become more sensitive and precise, it might become available for other types of cancers.
“Most of what we do now is in the context of bone marrow transplants and CAR T-cell therapy. But for lung cancer patients who get checkpoint inhibitors, we’re trying to evolve surrogate markers,” Dr. Maslak says. “Some of these tests are clinically available now and they’ll measure your lymphocytes. But in the future, you could basically see how these cells are being turned on and off. Maybe we’ll be able to measure those biomarkers and see how effective they’ve been, and we’ll be able to predict which type of checkpoint inhibitor you should get, because they’re all a little different in terms of response. What we’re researching now is trying to refine the response and predict what is the best agent to give a patient. It’s another form of personalized medicine.”
Immune monitoring and modification of treatment in response to the body’s reaction might also reduce toxicity to the patient overall while improving quality of life.
What makes Roswell Park different, and what brought Dr. Maslak here, is the close communication and partnership between doctors and researchers and the opportunity to work closely with scientific resources and core facilities that are instrumental in developing, refining and advancing new cancer treatments like immune monitoring.
“It goes back to the history of the laboratories here. We are on the cutting edge here at Roswell Park in terms of some of the instruments we’ve been able to secure and run. Some of this work is carried out in cooperation with other institutions, but not every cancer center has both sides, the medical and the research,” he says.
“In a place like Roswell Park, you have the physicians treating the patients, you have social workers helping the families of the patients, you have specialists who can talk to patients about fertility in the context of a transplant. It’s not compartmentalized.”