A key difference between chemotherapy and immunotherapy is that chemotherapy attacks cancer cells directly, while immunotherapy helps your immune system to fight the cancer. Because they work differently, your body reacts differently, and side effects may be different as well.
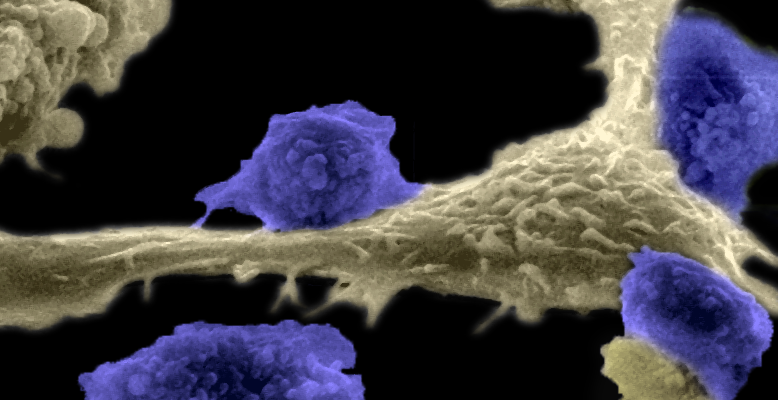
Your body’s normal immune response is to try to fight off invaders, such as viral and bacterial infections, and to rid the body of abnormal or mutated cells, such as cancer cells. But sometimes cancer can outsmart the immune system, shutting down its ability to detect or attack cancer. When cancer spreads into a healthy cell, it highjacks the DNA/RNA that control the cell’s functions, including division (reproduction). With the cancer cell’s DNA now running the show, every time the cell divides, it makes more copies of the cancer cell instead of the original, healthy cell. Without the immune system’s protective controls in place, the cancer is free to grow and divide uncontrollably.
How Does the Immune System Work?
Your immune system is made up of white blood cells and the organs and tissues of the lymph system. Its job is to protect you from infection, mutated (abnormal) cells and foreign agents. When you sprain an ankle, eat contaminated food or get stung by an insect, your immune system responds by sending white blood cells and other substances to the affected area. You may experience local swelling, vomiting/diarrhea or raised, red, bumpy skin. This protective response is called an inflammatory reaction. When this reaction goes into overdrive when there is no actual threat, you may develop an allergy or an autoimmune disease, such as rheumatoid arthritis, lupus or inflammatory bowel disease. If the inflammatory response is weak or doesn’t happen at all, you may wind up with an infection or other problem. Learn more about the immune system.
How Does Chemotherapy Work?
Traditional chemotherapy drugs attack cells that are reproducing very quickly. They interfere with the cancer cells’ ability to grow and divide, which damages or kills them. Because some normal cells in our bodies reproduce quickly, they, too, are attacked. This includes cells that line the digestive tract, hair follicles and bone marrow (where your blood cells and platelets are made). The damage to these normal cells causes some of the well-known side effects of chemotherapy, such as nausea, vomiting, diarrhea, mouth sores, hair loss and low blood counts. Low blood counts can cause fatigue and put you at higher risk for infection and bleeding.
How Does Immunotherapy Work?
The goal of immunotherapy, sometimes called biological therapy, is to help your immune system fight the cancer. This can be accomplished in a number of ways, and different classes of immunotherapy drugs work differently to activate the immune system or make it more effective. They may enable the body to make antibodies that mark the cancer cell for destruction, make cancer cells “visible” or vulnerable again, or insert a virus into the cancer cells. In CAR T-cell therapy, T cells (a type of white blood cell that fights infection) are removed and treated with special receptor proteins called chimeric antigen receptors (CAR). The receptor proteins make the T cells better at recognizing cancer cells. When the T cells are put back into the body, they attach to the surface of the cancer cells and activate and kill those cells.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!What Are the Side Effects of Chemotherapy and Immunotherapy?
The side effects of chemotherapy reflect how the drugs work — by attacking cells with a rapid rate of division. The side effects of immunotherapy reflect the way they work, too. Symptoms are similar to those you would expect when fighting off an illness. Here are some common side effects of immunotherapy.
- Skin problems: Redness, irritation, blistering, sun sensitivity (photosensitivity), dryness, rash
- Flu-like symptoms: Fever, chills, fatigue, weakness, dizziness; nausea/loss of appetite, body aches, sinus congestion, headache, shortness of breath, new/worsening cough
- Swelling of legs (edema), weight gain from retaining fluid
- Diarrhea
- Hormone changes, including low thyroid hormones (hypothyroidism)
Different classes of immunotherapy drugs have additional side effects.
- Immune checkpoint inhibitors: Rash, diarrhea and fatigue. Rare but potentially life-threatening side effects include allergic reaction and immune-mediated reaction. In an immune-mediated reaction, an organ, or organ system, becomes inflamed. Some examples include colitis (intestines), hepatitis (liver) and pneumonitis (lung). Immune-mediated reactions can also affect the nervous system, skin, eyes, kidneys, glands (hormonal imbalances), heart and musculoskeletal system.
- Examples: pembrolizumab/Keytruda® and nivolumab/Opdivo®
- Monoclonal antibodies: Skin and mouth sores (increased risk of infection), high blood pressure problems, heart problems. Some can cause capillary leak syndrome (fluid leaks from blood vessels into tissues), which can cause dangerously low blood pressure.
- Examples: rituximab/Rituxan® and trastuzumab/Herceptin®
- Immunomodulators: Blood clots, lowered blood counts, trouble breathing, mood/memory changes, birth defects, peripheral neuropathy.
- Examples: interferons, lenalidomide/Revlimid®, pomalidomide/Pomalyst® and IL-2.
- CAR T-cell therapies: Cytokine release syndrome (flu-like symptoms, usually mild to moderate, but they can be very severe), high or low blood pressure, neurologic changes (confusion, difficulty speaking or understanding, agitation, seizures, loss of balance, brain injury/disease), low white and red blood cell counts (increased risks of infection and anemia).
- Examples: tisagenlecleucel/Kymriah™ and axicabtagene ciloleucel/Yescarta™
Depending on your type of cancer, general health and other factors, immunotherapy drugs may be used alone, in combination with another immunotherapy, or with one or more traditional chemotherapy drugs. If your drug regimen includes both traditional chemotherapy and immunotherapy, you may experience side effects from both. Your provider will discuss all your treatment options with you.
Once a decision is made, a clinical pharmacist or nurse will meet with you to review the drugs in your treatment plan. This is a good opportunity to get answers to all your questions so you’ll know what to expect and can learn what you can do to prevent or minimize side effects. You can find tips on wellness and treating side effects in the booklet “Taking the Lead,” available in the patient education library in the patient portal, in the Resource Center for Patients and Families and in your clinic. If you did not receive this booklet in clinic, ask your nurse or pharmacist for a copy.