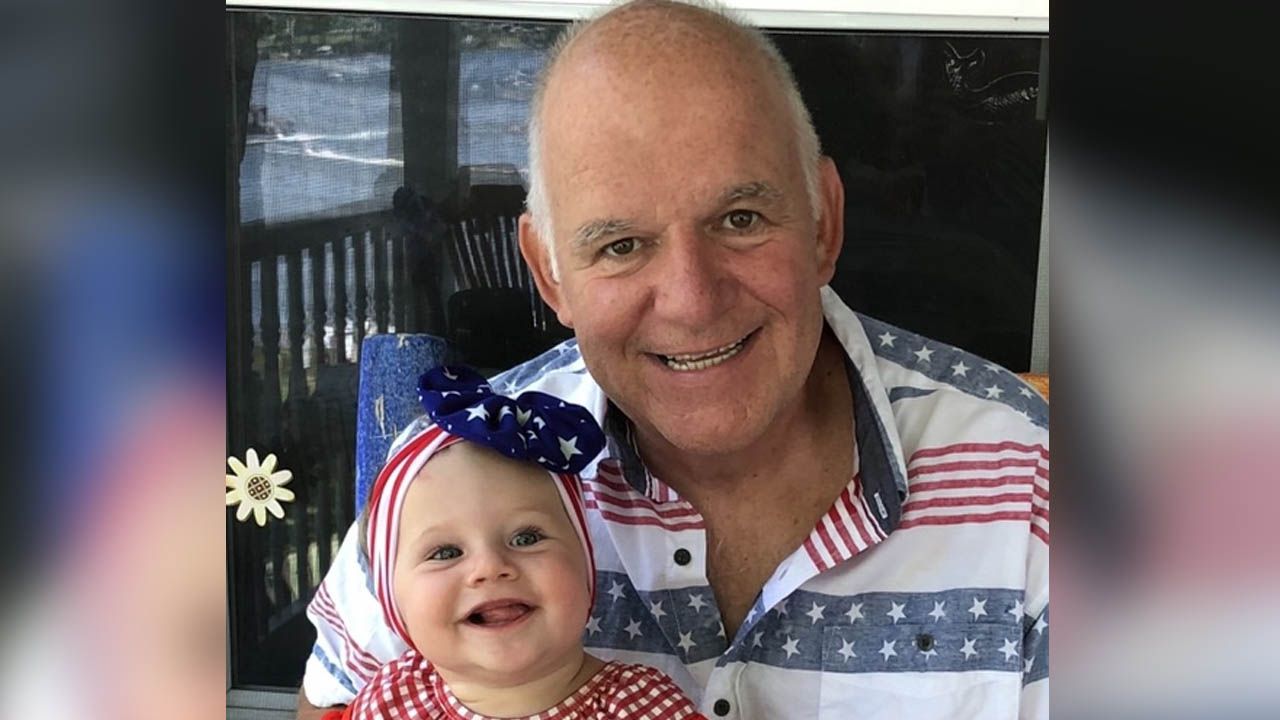
Prior to his 61st birthday, during the summer of 2019, Doug Green started having trouble swallowing.
"Food was getting stuck going down. It wasn't stopping me from eating, but it forced me to chew my food a lot more," says Doug.
By November, the problem persisted enough that his doctor scheduled an endoscopy to see what might be causing the issue. Doug assumed it was likely some common issue, such as GERD or acid reflux, but the test revealed he had stage 3 esophageal cancer.
"I was never a smoker, never a big drinker. I think it's possible my diet may have been a cause of my tumor, but the diagnosis was really a shock," says Doug. "I went in thinking they were going to find something that was minor, never considering it was going to be cancer. I was thankful my support network — also known as my wife — was in the room with me, because I don't think I heard a single thing after the word cancer. I saw the doctor's lips moving, but I'm not sure I heard anything after that."
A longtime engineer and plant manager for a Rochester manufacturing plant, Doug says much of his work is about finding solutions for complicated problems. So he took the same approach when facing his cancer diagnosis.
"On the day of diagnosis, I was scared to death, but the more reading and research I did, I began to understand that cancer is no longer a death sentence,” says Doug. “There is so much available treatment out there; you have to find the options and place that's right for you. I immediately wanted a second opinion, and that's why I called Roswell Park Comprehensive Cancer Center. They were very accommodating and got me in very quickly. Nine days later, I was at Roswell Park having a CT scan, and a few days after that, I met with the GI oncology department to discuss my options."
While meeting with his potential care team at Roswell Park, Doug was still considering options with the Rochester hospital that initially diagnosed his tumor.
Open vs. minimally invasive surgery
Doug's tumor was in a precarious spot known as the stomach junction, where the esophagus and stomach meet. To remove the tumor, Doug's surgeon in Rochester believed his treatment would require an open surgery, which would involve opening his torso from his chest down to his waist. However, his care team at Roswell Park had a different opinion.
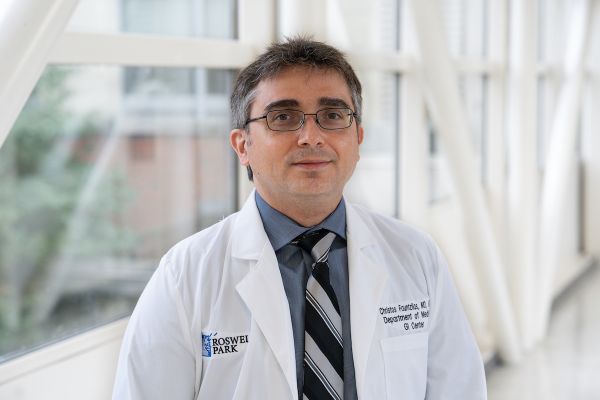
"For patients like Doug, their cancers involve the esophagus and stomach junction, and it is critical to determine the site of origin — where the tumor began — as it could originate in either the esophagus or the stomach, and choice of treatment and surgical approach would be very different," says Moshim Kukar, MD, FACS, Surgical Oncology.
“For surgery, you have to be in two different body cavities during this operation — in the belly and in the chest. Nationally, close to 50% of these procedures are still being done with an open approach, with big incisions on the abdomen and chest; the other 50% are attempting minimally invasive approach, which we prefer here at Roswell Park."
Research has found that minimally invasive surgery is associated with less risk of infection, less blood loss and faster recovery times. In recent years, many cancer centers have seen further benefits with this kind of surgery by using robot-assisted approaches in other disease sites. The adoption of minimally invasive approaches for esophagus and stomach tumors has been slow, given the complexity of these procedures.
"At Roswell Park, we treat 60 to 70 patients a year with gastroesophageal junction cancer, which makes us a high-volume treatment center for this disease,” says Dr. Kukar. “We have utilized minimally invasive laparoscopic approach for the last several years, but more recently we have begun to transition to a robot-assisted approach. The robot offers us 3D visualization, excellent control of the instruments that allow us to do a very precise oncologic dissection, with less trauma to the surrounding tissue. The robotic approach will lead to better outcomes, both for recovery and from an oncologic standpoint, and we are looking into this as we complete 100 robotic esophagectomies."
As Doug continued to consider his treatment options — to stay with a local general hospital in Rochester or travel to Buffalo to a comprehensive cancer center — his choice became clear.
"Based on the options of open vs. minimally invasive, it was an easy decision for me. More than that, I just felt very comfortable with the team at Roswell Park and having everything under one roof," says Doug. "I could meet with my oncologist, and if needed, it would take one phone call, and then I could see my radiologist all on the same day. It is just a very well-run team there, and all they do is cancer, so that's why I went with Roswell Park for my treatment."
Doug also had the opportunity to be a part of a clinical trial at Roswell Park to increase the odds that his cancer would be gone before surgery, which would improve his long-term survival rate. The treatment involved three rounds of chemotherapy before the standard mix of chemo and radiation, followed by minimally invasive surgery to remove the remaining tumor.
Yes, you have time for a second opinion
Like Doug, getting a second opinion could drastically change the course of your treatment. Roswell Park offers therapies and approaches unavailable from other providers.
Dr. Kukar and the Surgical Oncology team at Roswell Park removed the tumor, 16 lymph nodes and parts of Doug's esophagus and stomach. Despite this significant surgery, Doug was able to get up and walk around the hospital with minimal pain the next day. Tests showed clear margins after surgery. Next month Doug will return to Roswell Park for his six-month post-surgery CT scan to see if any cancer has returned.
"I'm very happy with the decision I made to be treated at Roswell Park. Despite the distance that I had to travel, I was happy to have everything I needed all at the same place. My oncologist, Dr. Sarbajit Mukherjee, Dr. Kukar and his surgical team, and all of the support staff there are amazing at what they do, and all they do is cancer,” says Doug.
"I'm definitely rethinking the next parts of my life. I'm rethinking my retirement plans after all of this, which is bittersweet, because my company was great to my family during my treatment, allowing me whatever time we needed. They even converted an office for me to take naps in while I was going through chemo."
Doug credits his wife as his primary support during his treatment.
"My wife's care and support have been unwavering through this whole thing, and we plan on traveling together a lot more when we're able to,” he says. “I'm starting work on my diet and exercise to help decrease my chances of recurrence and increase my odds that I will live to my normal life expectancy. I'd love to see my grandchild grow up. That would be an ideal thing.
"And with all the growing technologies and approaches to science, why shouldn't I?"
Editor’s Note: Cancer patient outcomes and experiences may vary, even for those with the same type of cancer. An individual patient’s story should not be used as a prediction of how another patient will respond to treatment. Roswell Park is transparent about the survival rates of our patients as compared to national standards, and provides this information, when available, within the cancer type sections of this website.