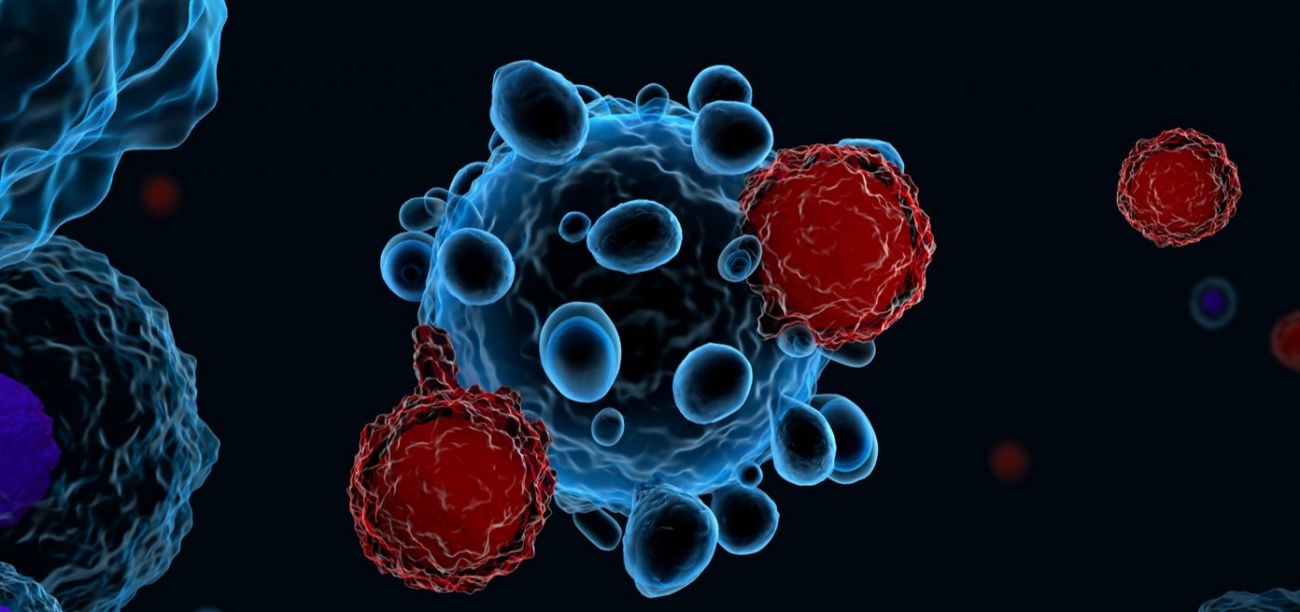
For many types of pediatric cancers, the treatment that helps save a child’s life might also cause lifelong challenges.
A revolutionary new kind of therapy might change all that.
Roswell Park Comprehensive Cancer Center was the first location in a 200-mile radius to offer CAR-T therapy for pediatric patients, using the child’s own immune system to help destroy cancer cells.
“CAR T cells are a revolution in the way we think about cancer therapies,” says Ajay Gupta, MD, MS, a pediatric oncologist at Roswell Park.
Acute lymphocytic leukemia, or ALL, is the most common form of pediatric cancer. It happens when bone marrow cells mutate and replicate out of control.
Patients with relapsing or refractory B-precursor acute lymphocytic leukemia (Pre-B ALL) have historically had an uphill battle against the disease, with a low rate of survival after treatment.
“With CAR T cells, now you have prolonged survival — many more of these patients are surviving. For the first time, it’s giving these patients hope and really changing the paradigm of how we think about cancer therapy,” Dr. Gupta says.
The important difference in using CAR T cells to fight ALL is that it is a targeted therapy, meaning it is more focused on the cancer cells, causing less damage to normal, healthy cells.
“You’re harnessing the immune system instead of beating it down and using it to our advantage against cancer,” he says.
A shapeshifting cancer
In CAR T therapy, the patient’s own T cells are adjusted to make them recognize the tumor cells again, turning the body’s immune system into an attack force once more. These cells are also better equipped at recognizing, responding to and expanding in the presence of cancer cells. The CAR T therapy that is currently approved specifically targets a molecule on the cell surface known as CD19.
To start on CAR T therapy, some of the patients’ T cells are removed from their bloodstream. “The T cells are sent off and DNA is put into the cell to recognize CD19 as a threat again,” says Meghan Higman, MD, PhD, a pediatric oncologist at Roswell Park. “The cells come back and they’re infused into the patient. What you’ve done is programmed the T cell to find the leukemia cell and kill that cell while telling other T cells to kill other leukemia cells.”
Patients are reinfused at Roswell Park and stay nearby at Oishei Children’s Hospital for observation “just to make sure we don’t have someone who doesn’t quite follow the pattern of side effects because our young patients might not be able to tell us if something’s bothering them,” she says.
Children who have been through one round of ALL treatment before and had a relapse might not be good candidates right away for a bone marrow transplant to fight their cancer a second, or third, time. “CAR T has an advantage in kids who have been heavily treated in that it’s still efficacious. CAR T treatment was able to put these kids back into remission,” Dr. Higman says.
Unlike chemotherapy and radiation, which have long-lasting side effects that can linger throughout the body, CAR T cells are a targeted treatment. Patients may still face the possibility of acute side effects from those therapies, including over-stimulation of the immune system, known as cytokine release syndrome, which physicians have learned over time how to manage well.
“CAR T cells targeting CD19 also can have manageable longer-term toxicity to normal immune cells that also express CD19, known as B cells, causing prolonged immunosuppression which is treatable with intravenous immune globulin, a kind of mixture of antibodies,” Dr. Gupta adds. This is a condition that lasts only as long as the engineered CAR T cells circulate in the body. Researchers are working on ways to keep CAR T cells alive longer to provide longer-term protection against ALL, as losing that “living drug” means a patient could relapse.
Treating pediatric leukemia
Find out the different ways Roswell Park doctors can treat pediatric leukemia.
Learn MoreTreatment close to home
Roswell Park has been offering CAR T-cell therapies for adult patients since 2018 and began the treatment with pediatric patients in 2020.
“CAR T cells are revolutionary for pediatric patients and Roswell Park was, until recently, the only hospital in the region to offer this,” Dr. Gupta says. “We’re still in the early days of CAR T-cell therapy but I think we will become a center for immunotherapies and new and novel ways to attack cancer using the immune system. Many patients who get this treatment respond well.”
That was true for Chasity, a young girl from Niagara Falls, NY, who was diagnosed with leukemia at just five weeks old. She had CAR T therapy before her second birthday, making her one of the youngest patients – and possibly the youngest – to receive CAR T therapy and go into remission from her cancer.
“We’re able to provide treatment in a seamless manner,” Dr. Higman says. “It’s available here and we can move patients relatively quickly and we will work with families as a team to bring their patients back home.”