“It’s so easy, I feel like I’m getting away with something.” That’s how Nella Smolinksi describes the last three years of treatment with an immunotherapy drug to control her rare form of Hodgkin lymphoma (HL).
But Nella’s cancer treatments weren’t always so easy. Her symptoms began in 2010, when her whole body began to itch intensely, although she had no rash. For three years, Nella went to several doctors to figure out a cause and cure, but to no avail.
Then, a few weeks before Nella learned that she was pregnant with her sixth child, her chiropractor noticed a lump on her neck. “I now know that both itching and swollen lymph nodes can be signs of Hodgkin lymphoma," says Nella. After running tests, her general physician referred her to Roswell Park, where she was diagnosed with mixed cellularity classical Hodgkin lymphoma.
When she was 20 weeks pregnant, Nella started chemotherapy treatments every other week for three months. In week 32 of her pregnancy, she delivered a healthy baby girl, and two weeks later, resumed chemotherapy for another three months. “Some days I was so tired and weak that I couldn’t get out of bed. But, I had a wonderful support network to help with the kids, and after those final three cycles of chemo, it appeared my cancer was gone,” she recalls.
Eighty-five percent of classic HL cases are cured (no evidence of returning cancer for at least five years) after the first line of treatment. But, six months after completing chemotherapy, Nella starting itching again. A PET scan and biopsy confirmed that her cancer had returned.
Stem Cell Transplant Provides Second Chance
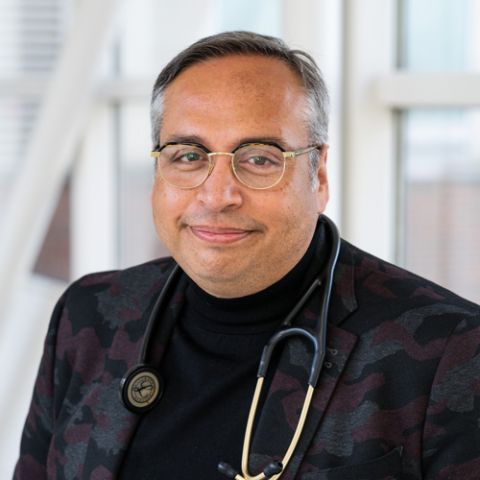
Treatment for patients with relapsed Hodgkin lymphoma is different, and more difficult: two cycles of chemotherapy, followed by high-dose chemotherapy and then an autologous stem cell transplant.” Nella’s doctor, Francisco Hernandez-Ilizaliturri, MD, Chief of Roswell Park’s Lymphoma Section, explains that in this lengthy process, "hematopoietic stem cells (immature cells that produce and form blood cells) from the patient’s blood are removed and frozen. Then, the patient’s bone marrow and the cancer cells inside them are destroyed with chemotherapy and/or radiation in a process called dose-intensive therapy. Next, the stem cells that were collected previously are thawed and given back to the patient intravenously. They travel through the patient’s bloodstream and back into the bone marrow, where they can start producing healthy blood cells again.”
Nella lived in Roswell Park’s transplant unit for 26 days. Because the area needs to be as sterile as possible, visitors are carefully screened. “The kids visited once, but it was very difficult, so we never tried that again,” she recalls. “However, my husband worked nearby and would stop over every day on his lunch break. My dad visited me nearly every day, and my siblings visited frequently. And my parents were able to help us with childcare.” After her discharge from Roswell Park, she spent another three weeks at her parents’ house, away from her children, to recover and limit her exposure to germs.
Three months after this grueling process, all symptoms of cancer were gone, only to resurface 21 months later. This time, she enrolled in a clinical trial in New York City. Her disease was kept at bay for about a year until she suffered a complication with her liver and she stopped the drug.
Eventually, it was determined that Nella had paraneoplastic cholestasis (PC), an extremely rare manifestation of HL that causes intense itching and reduced bile flow from the liver. Dr. Hernandez-Ilizaliturri notes that there are fewer than 20 published cases of this type of HL, and no reported cases in relapsed HL.
Roswell Park Division of Translational Immuno-Oncology
What is immunotherapy and how does it work? Our experts explain more.
Learn MoreImmunotherapy Offers New Approach
Back at Roswell Park, Nella received three doses of emergency inpatient chemotherapy, referred to as “bridge therapy, to get my liver back on track,” she says. Then she began treatment with an immunotherapy drug. Immunotherapy is a new approach in cancer treatment that uses the patient's immune system to fight the cancer. Cancer cells have adapted in order to hide from the immune system. Immunotherapies aim to unmask these cells so that immune cells can find and destroy them.
Nella began treatment with twice-a-month infusions of nivolumab (Opdivo®), a type of immunotherapy called a checkpoint inhibitor. “Essentially, the drug turns off proteins on the surface of cancer cells that act as an ‘invisibility cloak,’” she explains. “This allows my immune system to recognize and attack the cancer cells. While it took a few months to get my liver back to ‘normal,’ I noticed a change in how I felt almost immediately.” She has now successfully been on this therapy for three years, with no relapses.
“Nella’s case is the first reported successful treatment of a patient with this condition in the setting of relapsed HL after a stem cell transplant,” says Dr. Hernandez-Ilizaliturri.
After all that her treatment has involved, Nella believes her current plan is far easier. “I go to Roswell Park every two weeks to get my infusion. Occasionally I’ll get a rash, which is easily treated,” she says. “To look at me, no one would suspect I am living with cancer. I can work out, be an active parent to my children and spend time with family and friends. While I might never be ‘cured,’ all I need is to be able to live my life normally, and for the last three years, this type of immunotherapy has allowed me to do just that.”
Editor’s Note: Cancer patient outcomes and experiences may vary, even for those with the same type of cancer. An individual patient’s story should not be used as a prediction of how another patient will respond to treatment. Roswell Park is transparent about the survival rates of our patients as compared to national standards, and provides this information, when available, within the cancer type sections of this website.