Over 5 million Native Americans belonging to one of 567 federally recognized tribes currently live in the United States.
Although each tribe has its own unique history and culture, one thing all Native Americans have in common is an increased risk of cancer and other diseases, including diabetes, heart disease and obesity.
What’s even more concerning is that while the number of cancer deaths has begun to level off or decline in recent years thanks to advances in prevention, screening and treatment, more Native Americans are dying of cancer than ever before.
Why Are Cancer Rates Higher among Native Americans?
Many different cultural, economic and biological issues contribute to health disparities, or differences in the way cancer and other diseases affect individuals and communities. Despite tribal and regional differences, Native Americans overall have higher-than-average rates of most cancers and other co-occurring conditions, particularly gallbladder, stomach, liver and kidney cancer. Native Americans also have the lowest cancer survival rates in the country, mainly because they’re getting screened too late, if at all. Many forces are working together to create these cancer disparities, including:
- Living conditions. Compared to the rest of the population, Native American communities have much higher rates of poverty and lower levels of education, both of which have a big impact on health.
- Tobacco, drug and alcohol use. Native Americans have the highest rates of cigarette smoking in the country. They are also 10 times more likely to die of alcohol-related causes and twice as likely to die of a drug overdose than the average US resident.
- Obesity. Although rates of obesity vary widely among tribes — from 11% among Navajos in New Mexico to 80% of Pima-Maricopas in Arizona — Native Americans are more likely than members of many other ethnic groups to be overweight or obese.
- Diet. Certain foods, such as processed meat, can increase the risk of cancer. Colon cancer and stomach cancer are among the leading causes of death in Alaska Natives, whose diet is high in salty, preserved fish and low in fresh fruits and vegetables.
- Environmental contamination. Native communities and reservations tend to be heavily impacted by the agriculture, drilling and mining industries. Concerns over the Dakota Access Pipeline on the Standing Rock Indian Reservation in 2016, as well as the forcible eviction of the Seneca people during construction of the Kinzua Dam in the 1960s, are two examples of clashes between Native and Western cultures over environmental issues and land rights.
Addressing Health Disparities in Native Communities
To help reduce the cancer burden in Native American communities, we need to remove barriers to quality health care. Differences in access to services that prevent, detect and treat cancer are driving the higher rates of cancer in Native communities. Although many Native Americans have access to the Indian Health Service (IHS), the IHS is chronically underfunded. In fact, the federal government spends almost twice as much on health care for prisoners as it does for Native Americans.
To understand Native American cancer risks, we need an accurate picture of health at the tribal level. However, many studies report cancer rates among Native Americans as a whole or by IHS area. For example, cancer rates among the Haudenosaunee (otherwise known as the Iroquois) — a large group of about 125,000 Native Americans comprising the Mohawk, Onondaga, Oneida, Cayuga, Seneca and Tuscarora tribes — are often lumped in with those of the Penobscot of Maine, Seminoles of Florida, Cherokee of North Carolina, and every other federally recognized tribe in the Eastern United States, even though these tribes are vastly different in terms of diet, lifestyle, culture, and first contact with Europeans.
Here at Roswell Park, we are using many different approaches to look at regional cancer patterns among Native Americans, particularly the Haudenosaunee. Our goal is to see how we can work with Native tribes to better understand their unique health care needs. In 2016, we partnered with the IHS to enhance education, outreach and prevention efforts in Native American communities through improved patient care, summer research experiences for Native students, and community-based research.
We’ve also been working on various projects with Native Nations in our region, including a community health survey, pilot testing of a workplace module developed to address the problem of obesity and obesity-related cancers, efforts to engage Native communities in medical research and biobanking, and various educational programs. Roswell Park has a summer internship experience that gives students from various Native Nations the opportunity to participate in cancer research. Last summer, our interns translated cancer "tip sheets" into the Seneca language in the hope that it might generate more interest in cancer screening and prevention in the community.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!Overall, I’ve seen a resiliency among Native people moving toward healthier lifestyles. Many Native Nations are opening up to the idea of developing partnerships with medical institutions such as Roswell Park to improve access to health services. Each Native American tribe is unique, but we all share concerns about the health disparities in our community and are working together to overcome them.
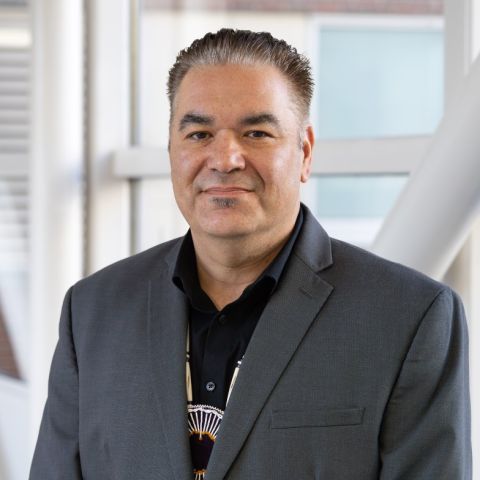
Dr. Haring is a member of the Seneca Nation of Indians and lives on the Cattaraugus Territory of the Seneca Nation of Indians. He is an appointed delegate to the American Indian and Alaska Native Health Research Advisory Council, which sets priorities and makes recommendations to the U.S. Department of Health and Human Services about Native American health research, programs and policies.