This condition typically occurs in people who suffer chronic gastroesophageal reflux disease (GERD). Over time, the tissue lining of the esophagus is replaced by tissue similar to what’s found in the intestinal lining. Determining which people with the condition are most likely to develop cancer — and should seek treatment — isn’t always clear.
Expert monitoring is essential
Anyone with Barrett’s esophagus should have a periodic upper GI endoscopy with a biopsy. A pathologist will examine the tissue sample to assess how abnormal the cells look, a condition known as dysplasia. The abnormal cells may be called high-grade (more likely to cause cancer) or low-grade (less likely to cause cancer). Having Barrett’s esophagus with high-grade dysplasia is considered a precancerous condition and most people should be treated in a timely manner.
Endoscopic treatments for Barrett’s esophagus
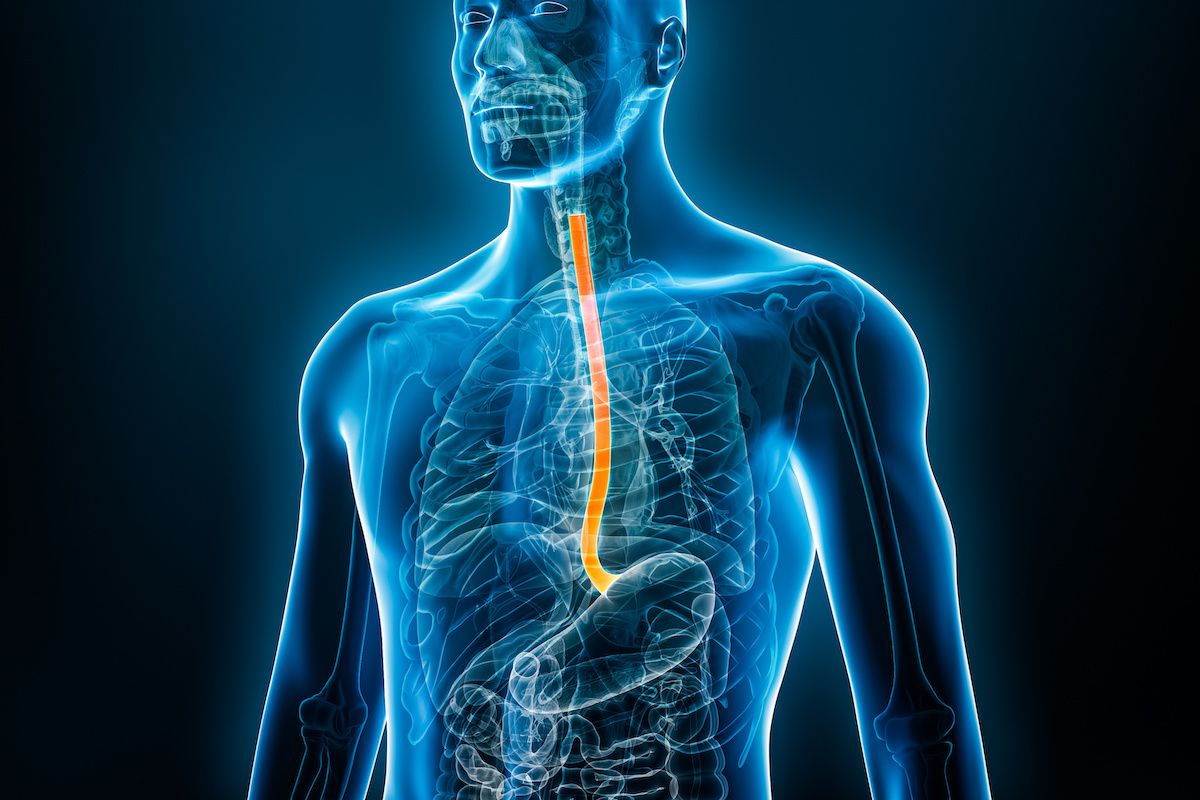
Roswell Park offers multiple options to treat Barrett’s esophagus without major surgery. These include endoscopic treatments that reach the diseased portion of the esophagus through the mouth with a device called an endoscope, a long thin tube outfitted with a lights, camera and specific tools to treat or remove abnormal cells. These treatments include:
Radiofrequency ablation (RFA) for Barrett’s esophagus
In this treatment, the endoscope is outfitted with a device that uses radio waves to heat the abnormal tissue. The abnormal or precancerous lining that has been subjected to this heat will eventually shed off and be replaced with tissue that is not precancerous.
Endoscopic mucosal resection for Barrett’s esophagus
This minimally invasive surgical procedure is often used to remove superficial abnormal lesions or tissue. The procedure involves lifting the Barrett’s lining and injecting a solution underneath or applying suction, and cutting the lining off, which is then removed with an endoscope.
Photodynamic therapy for Barrett’s esophagus
A non-surgical treatment that was pioneered at Roswell Park, photodynamic therapy (PDT) uses a light sensitive drug that concentrates in cancer cells. The drug causes cancer cells to die when activated by specific wavelengths (colors) of light applied with a laser beam. PDT treatment can be repeated as necessary.
The Photodynamic Therapy Center at Roswell Park is a worldwide leader in using PDT to treat cancers of the skin, mouth, larynx, esophagus, head, neck, lung, breast and some gynecological cancers.
New light-sensitive compounds have been developed by Roswell Park researchers for use in PDT treatment. One agent, called HPPH or Photochlor, results in a far shorter duration of the light-sensitivity side effect. Photochlor is currently being evaluated in clinical trials at Roswell Park for use in lung, head and neck cancers.