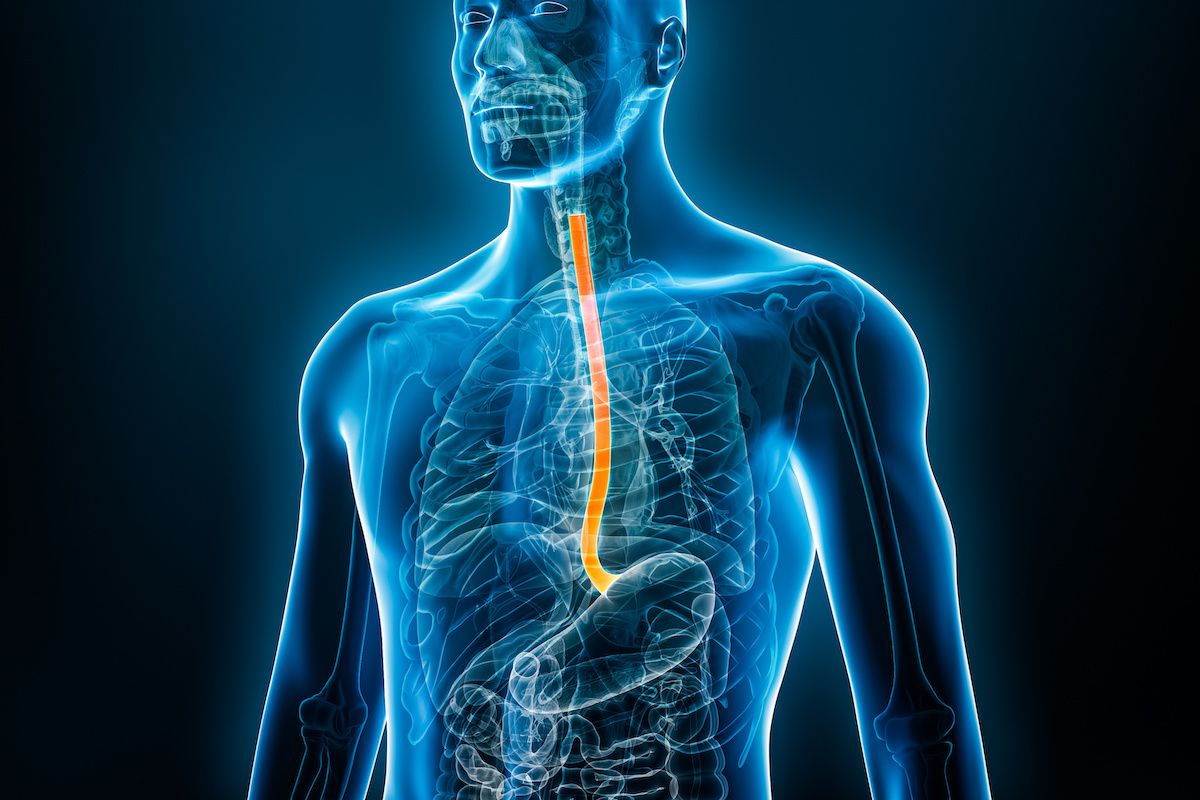
Acid reflux occurs when stomach acid leaks back up into the esophagus, causing heartburn, indigestion and other discomfort. Eating a large meal or acidic foods and drinks are all things that may cause irritation during the digestion process, and while acid reflux can be common, is there a point at which you should become worried about it?
When acid reflux becomes chronic, the name for this condition is gastroesophageal reflux disease, or GERD. Ongoing GERD may begin to cause damage to the esophagus lining, leading to a condition called Barrett’s esophagus.
Risk factors for Barrett’s esophagus
“Barrett’s esophagus is the esophagus’ response to chronic reflux,” says gastroenterologist Anoop Prabhu, MD, FASGE, formerly an Associate Professor of Oncology in the Department of Internal Medicine at Roswell Park Comprehensive Cancer Center. “The stomach creates copious amounts of acid to help with digestion, but the esophagus is not well suited to deal with that acid. In response to chronic reflux, the esophagus will often change its lining, and the name for that change is Barrett’s esophagus.”
While GERD is the strongest contributor for developing Barrett’s esophagus, there are additional traits that make a person more at risk for developing the disease, such as:
- White race
- Assigned male at birth
- Age over 50
- Smoking
- Obesity
- A family history of Barrett’s esophagus or esophageal cancer.
Since Barrett’s esophagus is relatively asymptomatic, many patients may not realize they have this condition. Typically, people learn that they have Barrett’s esophagus when they undergo an endoscopy for another reason, such as reflux, problems with swallowing, and chest discomfort or heartburn.
If Barrett’s is identified during an endoscopy, a biopsy is taken of the esophageal lining during the procedure to verify the presence of the condition.
Is Barrett's esophagus a cancer?
Barrett’s esophagus is considered a precancerous condition, however the vast majority of people with the condition do not develop cancer. On average, for every 1000 people who have Barrett’s esophagus, only three to five of them will be diagnosed with cancer.
The key determinant is whether there is dysplasia (abnormal cells), a sign of advanced stage Barrett’s. For people with high-grade dysplasia, meaning dysplasia that is very close to (but not quite) cancer, the chances of developing cancer increases — up to 15 to 20%. “If a patient shows signs of either low-grade or high-grade dysplasia, we’ll typically perform treatment to eradicate the Barrett’s condition, because we know that those individuals are at a higher risk for developing cancer than the average patient with Barrett’s.”
Why Roswell Park?
If you are diagnosed with a precancerous condition, it's important to be monitored in a center where the experts are.
Can Barrett’s esophagus be reversed?
Yes, says Dr. Prabhu. “Barrett’s esophagus can be treated to the point of eradication, which would reverse it all together. Similarly, medications can prevent it from progressing any further towards cancer.” Surveillance endoscopies are also performed regularly to assess the evolution of the Barrett’s — typically every three to five years after initial diagnosis.
Treatment and management of Barrett’s esophagus is proven to be effective in two different ways:
- Medications called proton pump inhibitors
- Ablation procedures, specifically radiofrequency ablation
“The first line management of Barrett’s esophagus is through proton pump inhibitors,” says Dr. Prabhu. “These are acid-reducing medications meant to decrease the damage of acid reflux and, as a result, decrease the rate at which Barrett’s esophagus converts to cancer.”
Through radiofrequency ablation, high amounts of heat are applied to the lining of the esophagus where Barrett’s is present. The lining that has been subjected to the heat will eventually shed and be replaced by tissue that is not precancerous. In some situations where Barrett’s has progressed to early cancer, there are still minimally invasive treatment options available via endoscopy. “We’re able to remove the cancer via the endoscope without surgery or chemotherapy, and provide a curative treatment with the scope alone,” says Dr. Prabhu.
It is for this reason that it is important to seek out expertise at a center that has the experience and volume of treatment for your disease. “There are data and guidelines supporting the idea that if you have advanced Barrett’s esophagus, you should go to a center of excellence where there are multiple specialists involved in your care,” says Dr. Prabhu.
Because of this expertise — and a care team that includes both a surgical oncologist and an endoscopic oncologist — your treatment plan will be customized to your unique disease.
"We’re able to remove cancers earlier," Dr. Prabhu says. "In individuals who could potentially have a surgery where part of their esophagus is removed, we may be able to save them from this surgery and perform an organ-sparing intervention.”