Roswell Park’s long history of cancer research has yielded many new discoveries and breakthroughs that became important milestones in the fight against cancer. We must always look beyond our discoveries in the laboratory to develop how this may help fight cancer — and how soon. Our patients are waiting.
81
U.S. patents
14
Biotech spinoff companies
101
License agreements
Key discoveries born from Roswell Park laboratories
A look at the game-changing innovations that were born at Roswell Park Comprehensive Cancer Center.
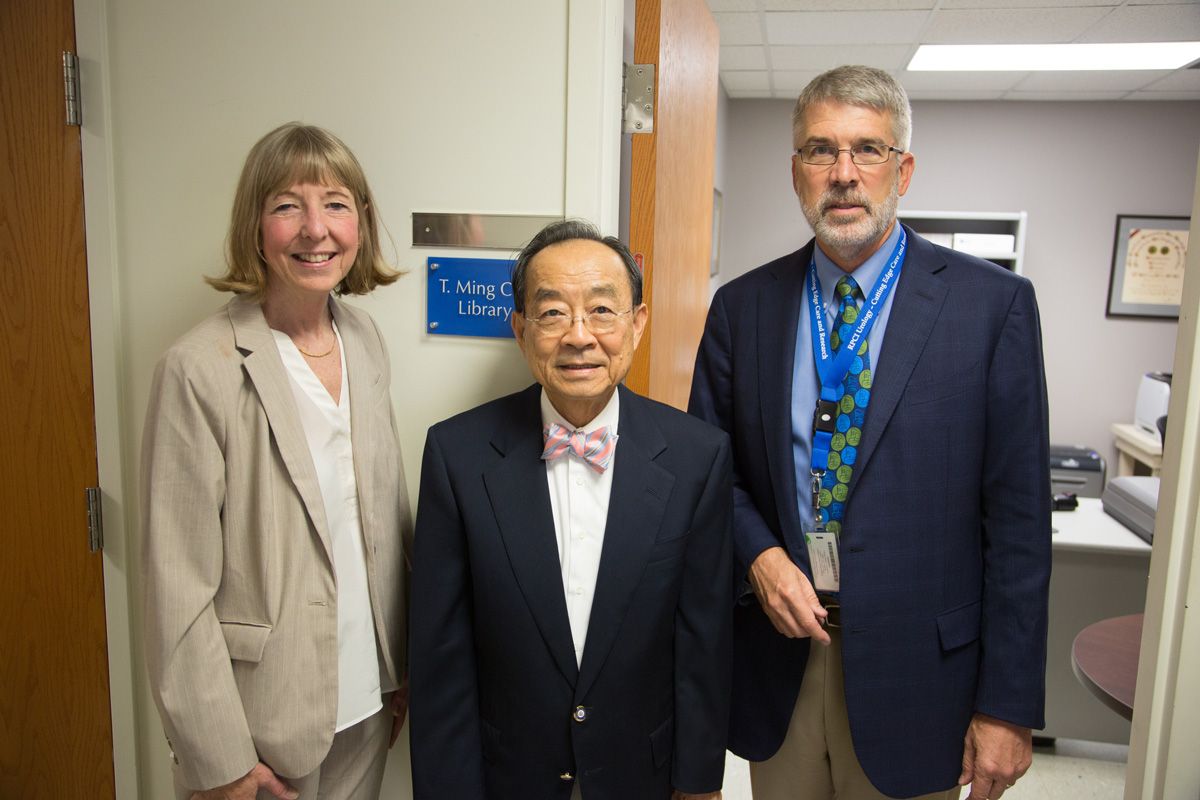
PSA screening test for prostate cancer
Roswell Park’s T. Ming Chu, PhD, DSc, discovered the prostate-specific antigen and developed the PSA test for early detection of prostate cancer. In 1986 the FDA approved the test for clinical use; it is now used worldwide. When the PSA test is used in men who fit the screening criteria, it reduces deaths from prostate cancer by 25-32%.
Breaking new ground in T-cell engineering
In a unique approach to cellular therapy, the Center for Immunotherapy launches the world’s first clinical trial using a two-gene combination for T-cell engineering. The clinical trial was led by Scientific Principal Investigator Richard Koya, MD, PhD, and Clinical Principal Investigator Kunle Odunsi, MD, PhD.
A vaccine for glioblastoma
Glioblastoma is an aggressive type of brain cancer with limited survival and few treatment options. A collaboration of Roswell Park neurosurgeon Robert Fenstermaker, MD, and scientist Michael Ciesielski, PhD, created a unique immunotherapy vaccine, SurVaxM, that targets survivin, a protein that helps cancer cells stay alive. A recent phase 2 study of 63 patients with newly diagnosed glioblastoma, demonstrated significantly longer survival time for patients treated with SurVaxM, with 93.7% alive a year after diagnosis, compared to expected 65% survival based on historical studies. The vaccine is being developed by Mimivax, and multicenter phase 2B studies are underway.
Genomic testing that matches a patients gene mutation with treatment options
OmniSeq TargetTM analyzes 23 different cancer-associated genes — such as ALK, EGFR, PTEN, KRAS and NRAS and more — to match patients with treatment options for their unique gene profile. Using multiple high-throughput genomic technologies, OmniSeq Target detects gene mutations, translocations, copy-number changes, and other alterations that are targetable, that can be addressed using the latest drugs and/or agents in clinical trials.
Polivy, a new drug for an aggressive form of non-Hodgkin lymphoma
The most common type of non-Hodgkin lymphoma, diffuse large B-cell lymphoma (DLBCL), is diagnosed in more than 18,000 people in the U.S. each year. Polivy is an antibody drug conjugate which means it combines a drug with a monoclonal antibody, a protein made in a laboratory that can zero in on a cancer cell, latch onto it, and either kill it directly or deliver chemotherapy or radioactive substances to kill it. Polivy targets CD79b, a protein made by most of the immune cells affected by B-cell lymphoma.
Back in the 1980s, Dr. Seon found a way to isolate CD79b, creating the antibody now called polatuzumab vedotin, and laying the groundwork for development of Polivy, manufactured by Genentech, Inc. Polivy was approved by the FDA in 2019.
Photodynamic therapy uses light to kill cancer cells
Developed by Roswell Park’s Thomas Dougherty, PhD, photodynamic therapy involves giving patients a light-sensitizing drug that accumulates in cancer cells but not normal cells. Then exposing the cells to a laser light causes a reaction that kills the cancer cells and shuts down blood vessels in the tissue around the tumor, reducing the chance that cancer cells left behind will be able to grow.
Roswell Park’s Photodynamic Therapy Center is a world leader in the use of PDT and offers the treatment for many skin, lung, gynecologic, esophageal, oral, head and neck cancers, as well as Barrett’s esophagus and other precancerous conditions or lesions.
Next generation photosensitizing drug
A new, second-generation light sensitizing compound called HPPH, or Photoclor®, was created at Roswell Park by Ravindra Pandey, PhD, Professor and Distinguished Member in the Department of Cell Stress Biology and Director of Pharmaceutical Chemistry. Previous photosensitizing drugs lingered in the body, necessitating that patients remain covered or indoors to avoid sunlight and bright artificial light for 4 to 6 weeks after treatment. Photoclor reduces the light sensitivity duration to 7 to 14 days.
A flight simulator to train surgeons in robotic techniques
A collaboration between the Center for Robotic Surgery at Roswell Park Comprehensive Cancer Center and the University at Buffalo (UB)’s School of Engineering and Applied Sciences produced the Robotic Surgical Simulator, or RoSS, to address the quickly growing need for a realistic training environment for robot-assisted surgery. The simulator provided a better training tool to perfect surgical skills and shorten the early learning curve of robot-assisted surgery without jeopardizing the safety and welfare of patients.”
The inventors founded the Western New York-based spin-off company, Simulated Surgical Systems, LLC to commercialize the simulators.
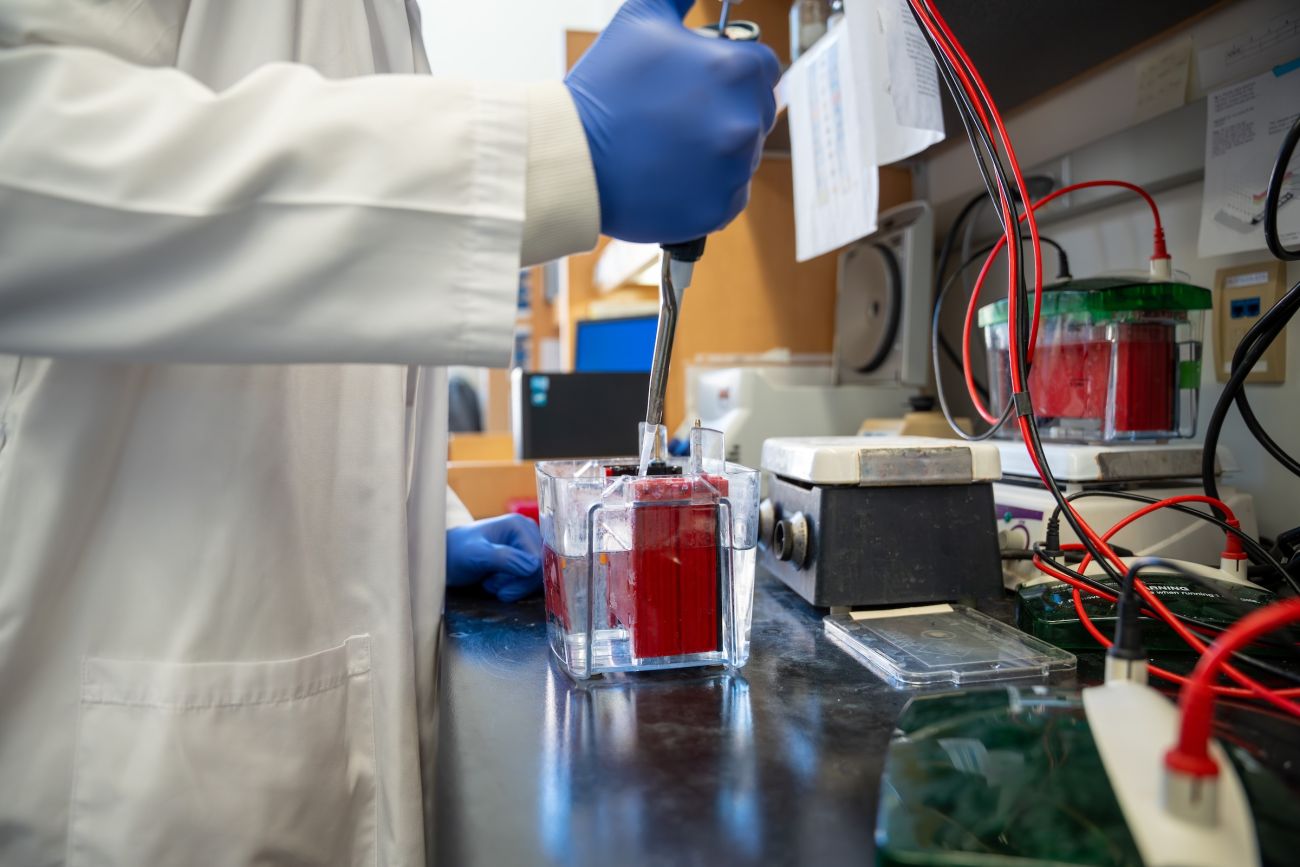
A laboratory essential for more than 50 years
In order to study cancer cells and how they behave, scientists must grow them in a laboratory. In 1966, Roswell Park researchers developed a new medium to help cancer cells grow and thrive — RPMI 1640, named for Roswell Park Memorial Institute. Today RPMI 1640 is manufactured by ThermoFisher Scientific on Grand Island, New York, and shipped to laboratories all over the world. It is also used to support tissue transplantation for burn and trauma patients.
Adding leucovorin to boost effectiveness of chemotherapy
In 1980, Roswell Park biologist Maire Hakala, PhD, observed that the chemotherapy drug 5-fluorouracil is more effective against cancer cells when leucovorin, a form of folic acid, is added. This information provides the basis for the development of 5-FU + leucovorin therapy, which later became the standard of care for treating colorectal cancer.