Roswell Park has two treatment vaccines in the arsenal against cancer; more in the pipeline
When most people think of vaccines, they think of the routine shots you receive as part of modern healthcare to help prevent serious illnesses such as measles, mumps, influenza, shingles, COVID and more, that are caused by a virus or bacteria. Cancer vaccines are different in that they can be used for both prevention and treatment, and use the body’s immune system to find and fight off cells that shouldn’t be there.
“A typical vaccine against a virus or bacteria is looking for cells that look very different in the body than your normal cells. But cancer derives from your own cells, which makes it hard for the immune system to find it,” says Igor Puzanov, MD, Senior Vice President for Clinical Investigation, Director of the Center for Early Phase Clinical Trials and Chief of Melanoma at Roswell Park Comprehensive Cancer Center.
Dr. Puzanov was a key investigator in the earliest research that led to FDA-approval of several breakthrough immunotherapy drugs, including pembrolizumab (Keytruda), nivolumab (Opdivo) and talimogene laherparepvec (T-VEC) for melanoma. At Roswell Park, he oversees all clinical trials, which are the heart of cancer research and future progress in cancer care.
Cancer vaccines are a form of immunotherapy
The vaccine that helps prevent influenza contains an inactive piece of a single protein of flu virus. This tricks the immune system into mounting a defense against the virus so that when the body encounters the flu virus, it knows what to do to fight it off.
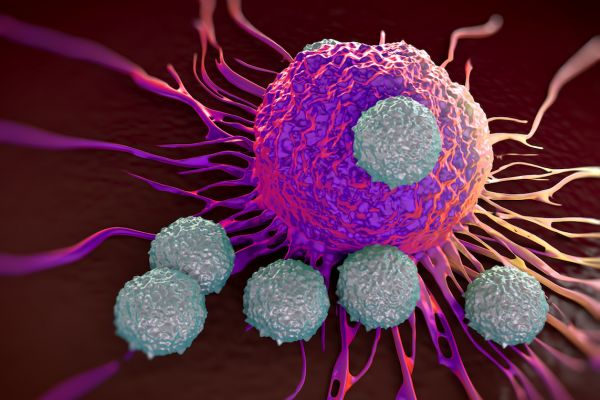
Cancer treatment vaccines use similar mechanisms to improve the immune system’s ability to fight off harmful cells. They use infusions or intratumoral injections of either modified cancer cells, parts of cancer cells combined with patients' healthy immune cells (dendritic cells) or pure proteins (called antigens). These may be specific to a certain type of cancer in general, such as glioblastoma , or to one patient at the time, which are personalized vaccines.
"Cancer treatment vaccines work like a piece of clothing with a scent that you give to a hunting dog. The dog will track the scent to its source and attack it. We are trying to train the immune system to recognize cancer, then find and destroy it,” Dr. Puzanov explains. “The trick is to find the right balance between stimulating the immune system and suppressing it.”
Making vaccines to treat an existing cancer is challenging on many fronts because cancer:
- starts in healthy cells that can “hide” the cancer cells from the immune system
- suppresses the immune system
- is difficult to destroy in large or advanced tumors
- is difficult to treat in people who are sick or older with a weakened immune system
However, advances in immunotherapy knowledge and technology have led to the development of dendritic-cell vaccines (DC vaccines) for some of the hardest-to-treat cancers, including pancreatic, melanoma, lung, breast and brain cancer. Currently available only through clinical trials, DC vaccines are used in combination with standard treatments such as surgery, chemotherapy and radiation.
“In order for cancer treatment vaccines to be successful alone, they should be administered as soon as possible after diagnosis, when the first cellular changes occur and the tumor burden is low,” says Dr. Puzanov.
How do dendritic cell vaccines work?
Dendritic cells are an important part of the immune system identified as professional antigen-presenting cells (APCs). They are highly mobile in the body, can migrate across impermeable barriers such as blood vessel (vascular) walls and are critical to presenting antigens on a cell surface to the fighter T-cells of the immune system. Dendritic cells are especially proficient in compelling T-cells to adapt their immune response to cancer- specific antigens and can be “loaded” with immunotherapy “cargo” — monoclonal antibody drugs like pembrolizumab and nivolumab — and deliver it to specific checkpoints on cancer cells to keep them from multiplying.
All vaccines incorporate some artificial stimulant to enable the immune system to respond against specific antigens (proteins) without making the host sick. “We are investigating a novel ‘two-signal’ theory to find a stimulant compatible with human T-cell antigen response that will train the immune system to attack a certain cancer or personalized cancer and remember that response,” Dr. Puzanov says.
Currently, Roswell Park has two cancer vaccines available to patients through clinical trials. A vaccine called SurVaxM was developed by neurosurgeon Robert Fenstermaker, MD, and scientist Michael Ciesielski, PhD, to treat glioblastoma, a rare and aggressive form of brain cancer. With standard of care therapies – surgery followed by chemotherapy and radiation — the median survival for people with glioblastoma is 15 months.
SurVaxM targets a protein called survivin found in glioblastoma cells and which helps keep the cancer cells alive. In phase 2 clinical trials, 63 patients with newly diagnosed glioblastoma received standard therapy plus SurVaxM. The study found the treatment was tolerated well and side effects were mild with low toxicity. Most promising — nearly all patients did not see their disease progress for six months and survival was extended for many. Some 51% of patients survived at least two years after diagnosis and 41% survived at least three years.
The study is now in phase 2B trials at 15 sites across the United States and China.
"Preliminary results suggest patients seem to be living longer with the novel treatment than with only standard glioblastoma treatment,” Dr. Puzanov says. "We have high hopes for advancement to an FDA-approved drug.”
Clinical trials of a cancer vaccine called *CIMAvax also are underway at Roswell Park for patients with certain lung and head and neck cancers. The trials are evaluating whether giving CIMAvax, along with the immunotherapy drugs pembrolizumab and nivolumab, can improve outcomes for patients with non-small cell lung cancer or squamous head and neck cancer. CIMAvax targets a protein receptor called EGFR, which aids tumor growth and development.
Another vaccine in the pipeline at Roswell Park has shown promise in the laboratory. This dendritic-cell vaccine appears to improve the effectiveness of radiation therapy against some aggressive and treatment-resistant forms of breast cancer.
“The rapidly developing science of immunotherapy may lead us to add these and other vaccines soon into our cancer-fighting armamentarium,” Dr. Puzanov says.
*Our first trials with CIMIvax have concluded. New trials are set to open soon.