Our gynecologic oncologists answer some of the internet's most-searched questions related to cervical cancer
When it comes to a gynecologic cancer, there are a lot of questions that might have you turning to the internet in search of answers. From screening to diagnosis and treatment, a cancer suspicion or diagnosis can send you down a rabbit hole.
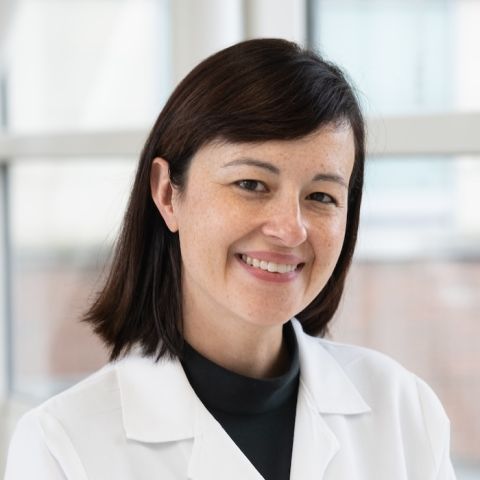
Roswell Park Comprehensive Cancer Center is here to help! Our gynecologic oncologists Katherine Mager, MD, FACOG, and Karen McLean, MD, PhD, FACOG, sat down to address some of the most frequently searched questions on the internet related to cervical cancer.
Are there symptoms of cervical cancer?
“The most common symptom is bleeding at irregular times,” says Dr. McLean. Other symptoms might include “bleeding in between your periods or bleeding after having intercourse, and occasionally pelvic pain.”
With the goal of catching cancers early, through screening tests like the Pap test, any symptom you may experience should be brought up to your doctor or gynecologist.
Is there screening for cervical cancer?
“There is screening for cervical cancer and it has evolved over time such that it now includes the Pap test, which is looking at the cells of the cervix, as well as HPV testing,” says Dr. McLean. “This is looking for subtypes of HPV, what we call high-risk strains, that may increase your risk of developing cancer.”
Your age and health history, as well as results from prior Pap tests, will determine how often you should be screened.
Will you get cervical cancer if you have HPV?
“A diagnosis of HPV is not a diagnosis of cervical cancer,” says Dr. Mager. “HPV, or human papillomavirus, is a very common virus that many adults will have had exposure to at some point, and the majority of people that have had an exposure will clear the infection on their own.”
This being said, HPV is associated with more than 90% of cervical cancers, so prevention of the development of cervical cancer is crucial — this is proven to be accomplished through vaccination. “The Gardasil vaccination protects against HPV and covers most of the strains associated with the development of cancer,” says Dr. Mager.
This vaccination begins around ages 11 or 12 and is routinely offered to everyone through the age of 26. Unvaccinated adults ages 27-45 should speak to their doctor about the benefits of getting the vaccine.
Why Roswell Park for cervical cancer?
All gynecologists on our cervical cancer team are board-certified gynecologic oncologists and leaders in their field.
What can cause an abnormal Pap test?
There are a few reasons why a regular screening test can be abnormal. “You can have an abnormal test because the HPV test is positive, but the cells of the cervix look okay,” explains Dr. Mager. “There can also be an abnormal test because the cells look abnormal, but the HPV is negative, or both can be abnormal.”
Dr. Mager stresses that an abnormal test is not a diagnosis of cancer. “Cervical infections or changes to the cervix that happen after menopause can also cause an abnormal Pap test result.”
Is cervical cancer genetic?
“I would say overall cervical cancer is not genetic,” says Dr. McLean. “It is almost always related to HPV infection, and that is not something you inherit from your family.”
Can cervical polyps be cancerous?
“Classically, cervical polyps are not cancerous,” Dr. Mager reassures us. “That being said, it’s really important that if there is ever a mass or a growth on the cervix, it needs to be biopsied and looked at under a microscope to confirm what it is.”
This is a minimally invasive procedure that can be done in your gynecologist’s office.
Is cervical cancer curable?
“Cervical cancer is, in general, highly curable,” says. Dr. McLean. “The biggest control for this is seeking regular care, like the Pap tests, HPV vaccination and catching it early if there is something going on.”