Fighting cancer always comes with certain costs to the patient — side effects, time, money and days lost to feeling unwell — but researchers at Roswell Park Comprehensive Cancer Center are trying to keep those costs low while improving the effectiveness of treatments against the cancer.
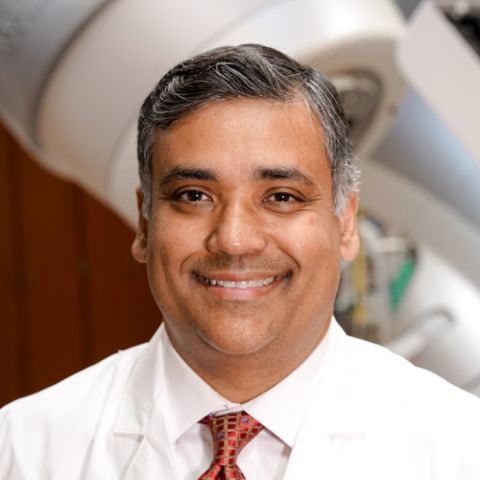
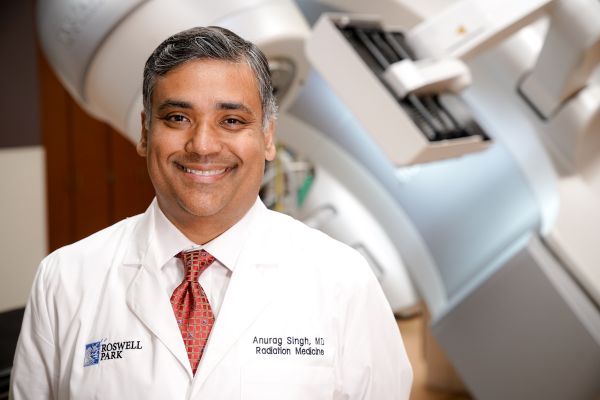
Anurag Singh, MD, Director of Radiation Research in the Department of Radiation Medicine and Co-Leader of the Cell Stress and Biophysical Therapy Program, and Emese Zsiros, MD, PhD, FACOG, Director of Research in the Department of Gynecologic Oncology, are among the Roswell Park doctors finding innovative ways to improve patients’ quality of life without sacrificing effective cancer treatment.
Dr. Singh has developed a new method for treating lung cancer with a single fraction of radiation treatment, instead of up to seven weeks of smaller doses, with reduced side effects for patients.
“You can use much more specific targeting if you’re only doing it once as opposed to smaller doses over seven weeks,” he says. The treatments can be administered with more precision, targeting the exact location of a tumor, which leads to more effective treatment and allows the patient to make fewer trips to the hospital for care.
“I became really excited about this over the last 15 years. There are equivalent outcomes of survival if you do stereotactic ablative body radiotherapy (SBRT) in either one, three, four, five or eight treatments, versus conventional radiation therapy over seven weeks. The really exciting thing now is something we weren’t aware of back then: immunotherapy.”
Dr. Singh and his team found that patients treated for metastatic cancer who are also getting immunotherapy might need a different approach to radiation so it will be effective in fighting their illness. Targeting multiple sites with precise doses of radiation therapy can reduce the number of overall treatments required.
“Take a young patient who has five sites of metastases. Single-fraction treatment makes a lot of sense,” Dr. Singh says. “Compare that to five treatments on each site, which leads to 25 total treatments for the patient. That is a lot more time and financial burden to the patient than five total treatments with single fraction.”
Dr. Singh’s studies have shown that “you can increase the number of immune cells in the tumor itself, and those on the periphery, meaning that targeted radiation treatments in combination with immunotherapy makes a lot of sense. We were the first to demonstrate that in people.”
This treatment program was recently supported by the European Society for Radiotherapy and Oncology (ESTRO), in the form of a recommendation within a consensus statement, and the American Society for Radiation Oncology (ASTRO) on management of patients with lung cancer during the COVID-19 pandemic.
Preventing painful mucositis
In addition, Dr. Singh has led research into the effectiveness of an anti-seizure drug, gabapentin, in treating mucositis, painful mouth sores that can develop in patients treated for head and neck cancers. Typically, patients with mucositis have been treated with opioids.
Mucositis often develops in patients receiving radiation and chemotherapy. Sometimes the pain is so great that patients ask to take a break from treatment. Unfortunately, those breaks can reduce the overall efficacy of treatment, Dr. Singh says. “Every day you break, our chances of curing you can be reduced by 3-5%. Sometimes we have to do double treatments to keep things on track.”
After an initial study using a rinse consisting of an antihistamine, a coating antacid and a local anesthetic, it was determined that this routine helped patients get through their initial treatment without needing a break. But after the first few weeks, the pain can become so great that some patients need a narcotic pain killer to continue.
Providing a preventive dose of gabapentin before treatment began resulted in patients needing narcotics only half the time, and those who did receive a low dose of methadone as a pain killer needed only about half as much overall as those who received fentanyl, which is highly addictive.
“We showed that those who got methadone instead of fentanyl had better quality of life and less pain. As a bonus, there are fewer narcotics in the system, because 50% of people won’t need narcotics. It’s a win-win-win.”
The National Comprehensive Cancer Network has adopted this recommendation as part of the NCCN Clinical Practice Guidelines in Oncology for Head and Neck Cancers, citing a 2019 study from Roswell Park that was led by Dr. Singh.
Giving ovarian cancer patients more — and better quality — time with their loved ones
Dr. Zsiros has spent the past several years researching the use of a three-drug combination in women who are fighting metastatic recurrent ovarian cancer, helping them improve the quality of their lives and, in some cases, giving them more time.
Two of the medications, Avastin and Cytoxan, have been given to ovarian cancer patients for the past 15 years. A newer drug, the checkpoint inhibitor Keytruda, has been approved for solid tumors but not for regular use against ovarian cancer. “The rationale was that Avastin helps to normalize tumor vessels so the immune cells can get into the tumor better. Typically, immunotherapy doesn’t work well for ovarian cancer, because often there aren’t immune cells inside the tumor.”
When used together, however, the three drugs help immune cells get inside the tumor to fight the cancer cells, providing patients who had been looking at palliative care the chance for longer survival.
This work was highlighted in JAMA Oncology last fall.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!“Our overall response rate was 47.5%. Historically, using these drugs independently, the rate was 8-15%. The combination has a synergistic effect,” Dr. Zsiros says. “The typical treatments for ovarian cancer compromise the quality of life. These patients would normally get chemo, which makes them feel terrible, but they do it because they hope their tumors will shrink and they will have more time. The beauty of this trial was not just the efficacy of the treatment, but there were barely any side effects. Patients had a really excellent quality of life.”
Following up on the patients involved in the trial, Dr. Zsiros and her team found they were happier, had great energy and a better emotional well-being in addition to an improved self-image. “They didn’t have that before,” Dr. Zsiros says.
She’s building on this research with another trial, examining tissue samples collected from patients to understand why the patients who responded best to this treatment did so well. While the original trial ended three years ago, she continues to administer the three-drug cocktail to ovarian cancer patients, as Keytruda’s manufacturer has approved it for compassionate care, meaning it is free to patients. To date, more than 100 patients total have been given this treatment at Roswell Park, and Dr. Zsiros is working to secure funding for a phase 3 trial. Avastin and Cytoxan are approved for ovarian cancer under the NCCN guidelines.
“The past few years we’ve seen great results. We really believe these patients had a great outcome and we continue to use it,” she says. “It’s become one of the Roswell regimens we offer to patients.”