The majority of people with prostate cancer — nearly 80% — are diagnosed early and cured by their treatment, most often radiation or surgery.
But one in five of those diagnosed with prostate cancer has a more aggressive form of the disease. Even before the individual has received any treatment or experienced a recurrence, doctors can identify whether the cancer is likely to be more dangerous and aggressive.
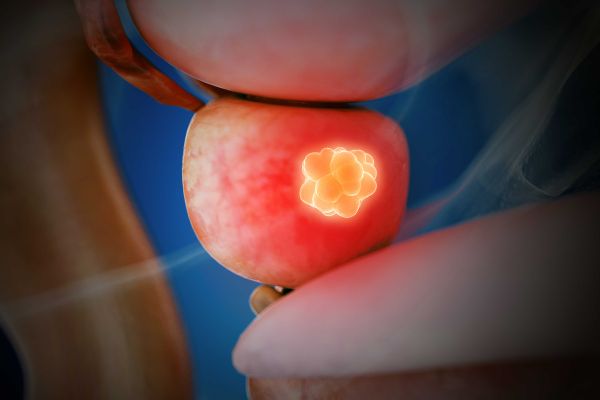
Prostate cancer is determined to be high risk if it is distinguished by any of the following characteristics:
- A larger primary tumor (greater than or equal to 4.1 to 6 cm, the size of a stage T3 tumor)
- A prostate-specific antigen (PSA) blood test result higher than 20
- Very abnormal cells in the prostate biopsy when looked at under a microscope, placing the cancer at Gleason grade 4 or 5.
Physicians perform biopsies or take X-rays to determine a cancer’s grade and stage. The stage is based on the size of the primary tumor or the extent it has spread in the body. The grade describes the appearance of the cancer cells and tissue under a microscope: the more abnormal they are, the higher the grade.
What are the main treatment options for people with aggressive or high-risk prostate cancer — and can the sequencing, or order in which different treatments are given, make a difference in overall effectiveness of these therapies?
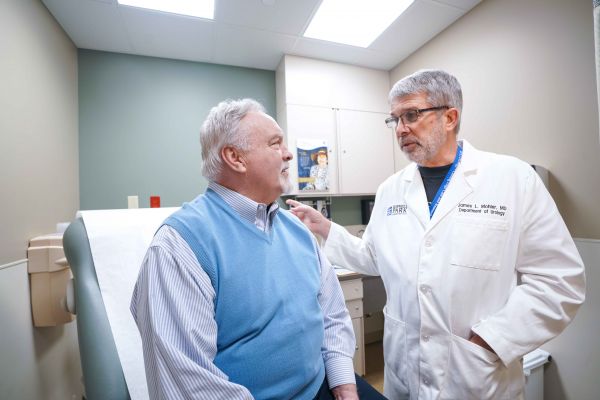
Roswell Park’s James Mohler, MD, Chair Emeritus of Urology, and Saby George, MD, a medical oncologist specializing in genitourinary cancers, were among the leaders of an Alliance for Clinical Trials in Oncology study that sought to determine whether aggressive treatment — having chemotherapy and hormonal therapy prior to surgery — would make surgery more effective, thus allowing patients to avoid the need for post-surgery radiation, also known as adjuvant radiation, and later hormonal therapy.
Why Roswell Park for Prostate Cancer?
Find out what makes Roswell Park unique in treating prostate cancer.
Learn More“Unfortunately, there was not enough benefit observed from this aggressive treatment compared to having only surgery immediately to warrant the adoption of this approach as a standard of care,” says Dr. Mohler, who is also Chief of Inter-Institutional Academics. “So we can’t conclude that more aggressive therapy leading up to an operation might be better for some patients.”
Dr. Mohler’s team found that delaying surgery in order for patients to receive these additional treatments in advance did not improve outcomes — evidence that prostate cancer patients and treatment teams should factor into treatment decisions.
“The bottom line,” says Dr. Mohler, “is that if a patient has high-risk prostate cancer, they should either have hormonal therapy and radiation or undergo surgery right away, without delay.”