The myelodysplastic syndrome (MDS) — also sometimes called preleukemia or smoldering leukemia — is a type of blood cancer in which mistakes in the bone marrow stem cells result in abnormal production of blood cells, including erythrocytes (red blood cells), leukocytes (white blood cells) and platelets. The abnormal stem cells do not develop or work properly, and often are destroyed either before they leave the bone marrow or shortly after they enter the bloodstream.
Some patients with MDS have too many young, immature blood-making cells in the bone marrow. When more than 20% of the bone marrow is made up of these cells, the disease is said to have transformed into acute myeloid leukemia (AML). This happens in about 30% of cases.
Because the diseased bone marrow stem cells don’t work normally, they don’t produce enough healthy blood cells of different types, which causes anemia and fatigue in many patients with MDS. Patients with MDS might also bruise or bleed easily due to low platelet counts, and they can be at increased risk for fevers or infections, because the bone marrow makes too few infection-fighting cells.
Normal blood cells
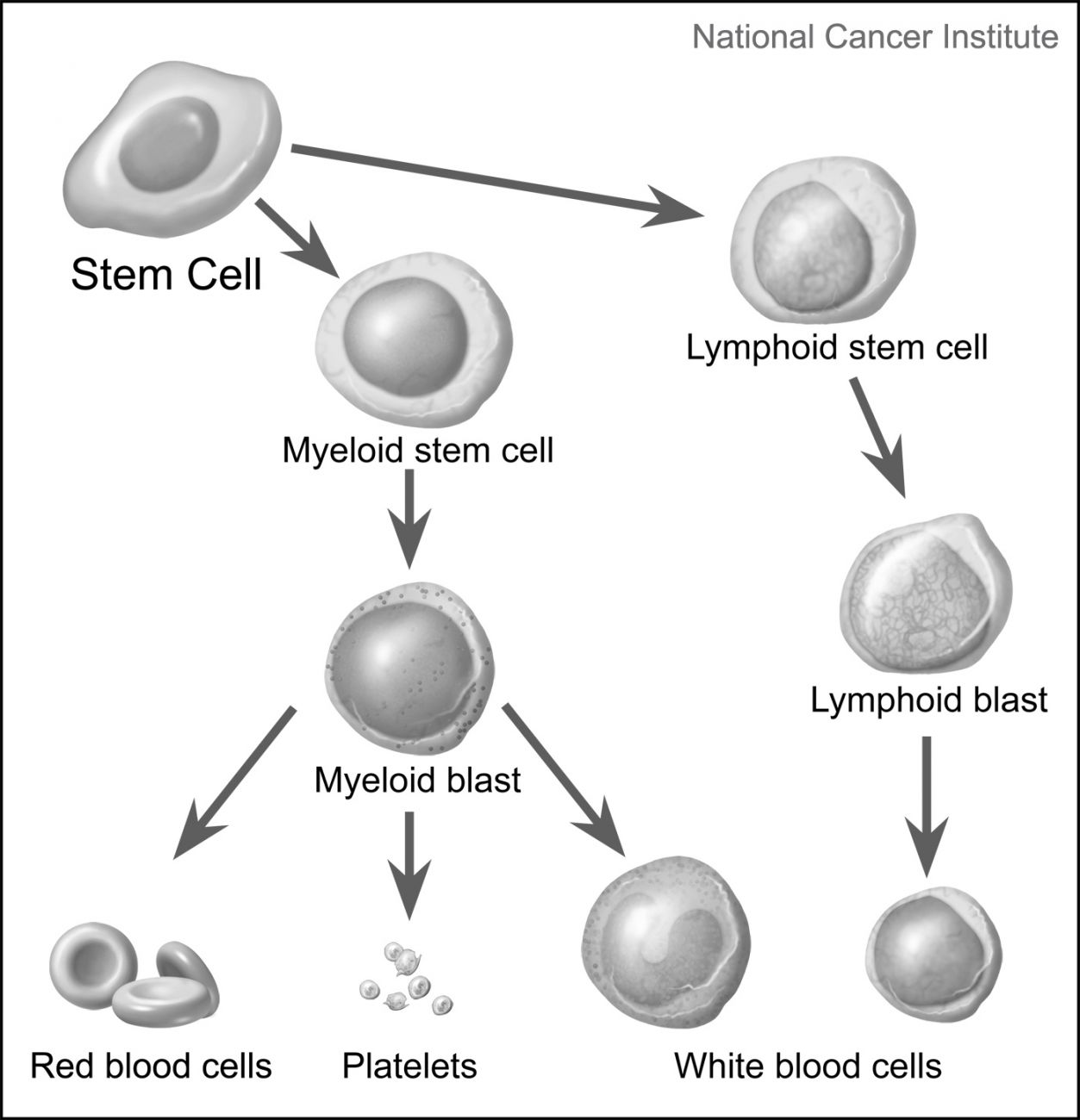
Most blood cells develop in the marrow, the soft material at the center of your bones. Bone marrow contains hematopoietic stem cells — immature cells able to develop into all the different kinds of blood cells — depending on the kind your body needs at a particular time. When cells grow old or are damaged, they die, and the hematopoietic stem cells replace them.
Stem cells mature into either myeloid stem cells or lymphoid stem cells.
- A myeloid stem cell matures into a myeloid blast, an immature blood cell that can turn into a red blood cell, platelets or one of several types of white blood cells.
- A lymphoid stem cell matures into a lymphoid blast, an immature blood cell that can turn into one of several types of white blood cells, such as B cells or T cells.
Each type of blood cell has a special job:
- White blood cells help fight infection. There are several types of white blood cells.
- Red blood cells carry oxygen to tissues throughout the body.
- Platelets help form blood clots to control bleeding.
MDS cells
In a person with MDS, the bone marrow makes immature blood cells (blasts) that do not work properly and remain clustered in the bone marrow.
Some MDS patients have an unusual feature — the presence of immature red blood cells that contain too many iron granules, called sideroblasts, that form in a ring.
Types of MDS
There are many subtypes of myelodysplastic syndromes, which are classified according to the number of blasts in the bone marrow, and the presence of ringed sideroblasts and specific chromosome abnormalities in the blood and bone marrow. If you have a higher percentage of blasts, you have a greater chance of developing acute myeloid leukemia (AML).
MDS subtypes include:
Refractory Anemia (RA)
About 8-15% of MDS cases involve refractory anemia. MDS patients with refractory anemia have low numbers of red blood cells, and those cells don’t look normal. The number of immature cells (blasts) in the bone marrow is usually normal (less than 5%). A small percentage of the red blood cells in the bone marrow (less than 15%) may contain sideroblasts (iron granules that form a ring).
Refractory Anemia with Ringed Sideroblasts (RARS)
Between 1.5-11% of MDS cases involve RARS. RARS has the same characteristics as refractory anemia (above), except that the number of ringed sideroblasts is more than 15%. Recently a new medication (luspatercept/Reblozyl®) was approved for patients with anemia and increased ringed sideroblasts.
Refractory Anemia with Excess Blasts-1 (RAEB-1)
In RAEB-1, there are not enough of one of the three types of blood cells, and those cells don’t look normal. The number of blasts is greater than 5% but less than 10%. About 18-21% of MDS cases involve RAEB-1.
Refractory Anemia with Excess Blasts-2 (RAEB-2)
This is the same condition as RAEB-1, except that the number of blasts is greater than 10% but less than 20%. RAEB-2 accounts for about 15-18% of MDS cases.
Myelodysplastic Syndrome, Unclassified (MDS-U)
Patients with MDS-U do not have enough of one of the three cell types, and abnormal white cell and platelet progenitor cells (a stage between stem cells and mature cells) are present. The number of blasts is less than 5%. Between 0-18% of all MDS cases involve MDS-U.
MDS Associated with Isolated Deletion (5q)
Patients have only refractory anemia (anemia that does not respond to treatment), but part of a specific chromosome — chromosome 5 — is missing.
RCMD Variations
The next two types of MDS — variations of Refractory Cytopenia with Multilineage Dysplasia, or RCMD — account for between 32-39% of all cases of MDS:
Refractory Cytopenia with Multilineage Dysplasia (RCMD)
In RCMD, there are not enough of at least two of the three different types of blood cells (red blood cells, white blood cells or platelets), and at least two of the blood cell types do not look normal. The number of blasts is less than 5% and the number of ringed sideroblasts is less than 15%.
Refractory Cytopenia with Multilineage Dysplasia (RCMD) with ringed sideroblasts
This condition is the same as RCMD, except that the number of ringed sideroblasts is higher than 15%.