New classes of drugs, new ways to use them before and after surgery
Learning you have cancer of any kind is life-altering; A diagnosis of lung cancer can be especially daunting, given it’s one of the five most difficult cancers to treat.
But advancements in therapeutic drugs and novel ways to use them — before surgery and/or after surgery, and in new combinations with established standards of care — are improving survival rates even for people with aggressive lung cancers.
While surgery has traditionally been the first line of defense for lung cancer, using systemic therapies (drugs that circulate through the whole body) such as chemotherapy, immunotherapy or targeted therapy before surgery, called “neoadjuvant” therapies, have become a successful standard of care for early-stage non-small cell lung cancer.
The goal is to shrink a tumor or kill cancer cells that may have already spread before surgery in order to increase the success rate of cancer-free survival after surgery.
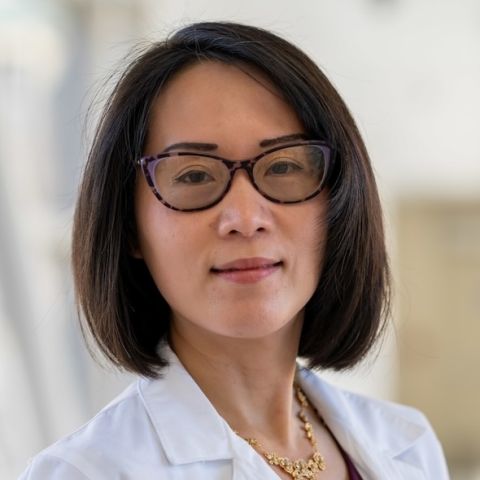
“Neoadjuvant therapy is to help improve the success rate of a cure before surgery is performed. Eligible candidates should have cancer that can potentially be cured by surgery, which is the primary therapy for lung cancer,” explains Grace Dy, MD, Director of Translational Research for Thoracic Medicine at Roswell Park Comprehensive Cancer Center.
“Biomarker testing is critical in determining the best systemic treatment option,” she says.
Expanding options beyond chemotherapy
Also known as tumor, molecular, genomic or genetic testing, biomarker testing looks for changes in the DNA/RNA of a tumor, including mutations, deletions, insertions and rearrangements of the DNA/RNA sequence. Biomarker testing can also look for levels of certain proteins, the amount of tumor DNA/RNA in the blood and missing or extra copies of genes.
Depending on the location and characteristics of the tumor, neoadjuvant therapy may be administered as a combination of intravenous chemotherapy and radiation, and some patients benefit from a combination of chemotherapy and immunotherapy, specifically checkpoint inhibitor drugs that target anti-PD1/PD-L1 antibodies.
New data indicates that this approach is more efficacious, less toxic, delays cancer recurrence or progression and improves overall survival in the treatment of advanced lung cancers.
“If neoadjuvant therapy is indicated, multidisciplinary review by the surgical, medical oncologists and the radiation medical team is important to determine the best neoadjuvant therapy to be administered. Patients are encouraged to review clinical trial options and eligibility with their treating doctors,” advises Dr. Dy.
New classes of cancer drugs
Novel lung cancer therapies over the last few years are on track to become “practice changing and paradigm changing,” reports Bailey Fitzgerald, MD, a Roswell Park medical oncologist.
“There are new approaches that didn’t exist five or 10 years ago. It’s hard to say looking out right now what’s going to be the thing that is the most practice-changing. But when you look at therapies for lung cancer in the past, especially small cell lung cancer, just the FDA approvals alone show that things have really, really changed,” she says.
“There are new classes of molecules that haven’t necessarily changed the game yet, but are really promising and exciting, like bispecific T-cell engagers.”
Bispecific T-cell engagers and antibody drug conjugates are on the front line of new treatments for advanced lung cancer. At Roswell Park, these two novel classes of drugs offer new options for people with lung cancers whose therapy may be otherwise limited.
You have time for a second opinion
A second opinion from a multispecialty team that focuses on lung cancer every day is important — we will ensure you get it without delay
Bispecific T-cell engagers offer new hope
Bispecific T-cell engagers (BiTEs), a type of immunotherapy, are providing new hope for people with treatment resistant lung cancer. The drugs are called bispecific because they have two targets: one on the body’s immune T cells, and one on the cancer cell, which brings the immune cells into close proximity with the cancer cells, enabling the immune cells to recognize and destroy the cancer cells.
In May 2024, the FDA gave accelerated approval to the bispecific T-cell engager Tarlatamab for treating small cell lung cancer, which often has a poor response to immunotherapy.
“This is the big story. It’s provided real efficacy for people with relapsed small cell lung cancer,” says Dr. Fitzgerald.
“When we have a breakthrough in any therapeutic, the first generation is really exciting, but the second, third, fourth generation with these types of drugs often tend to build on that success. It has been exciting to be able to offer the new treatment at Roswell Park because the new drug is showing efficacy in people whose cancer did not respond well to standard therapies,” she adds. “There’s been a huge effort across the institution to allow it to happen, from the immunotherapies team to the pharmacy to the hospital. This is a new medication, and it requires a highly specialized administration and monitoring,” says Dr. Fitzgerald. “It’s really been a coordinated effort across departments here at Roswell Park.”
Antibody drug conjugates — a new way to deliver cancer-killing agents
Antibody drug conjugates are engineered to recognize and bind to a specific protein or receptor on the surface of a lung cancer cell – and then deliver a payload of potent chemotherapy directly into the cancer cell. Once released, the chemotherapy drug kills the cancer cell, either directly or by triggering a series of events that leads to cell death.
“The idea is to be able to hone chemotherapies to specifically to cancer cells to allow higher efficacy with less toxicity on the organs and rest of the body,” explains Dr. Fitzgerald.
These new drugs can potentially transcend the limitations of traditional chemotherapy, including the need for high doses and potential side effects, and can more precisely target specific cancer subtypes. The choice of the chemotherapy payload should be carefully considered to balance potency and toxicity. Antibody drug conjugates are not suitable for all lung cancer patients, and l patient selection based on tumor characteristics and disease stage – determined by biomarker testing – is critical.
“The idea of the antibody drug conjugate is to provide options for people, especially patients with advanced or metastatic disease,” Dr. Fitzgerald says. “Dr. Dy has a couple of clinical trials open right now for some of these antibody drug conjugates, and has been a leader in bringing them to patients here at Roswell Park.”
Why Roswell Park for lung cancer?
The new paradigm in the treatment of lung cancer is to offer a personalized approach for each patient — determining the optimal treatments and best sequence of administering them based on each patient’s individual tumor.
“I would say the benefits of Roswell Park specifically are that it’s a comprehensive cancer center. All parts of the team work together closely and routinely, so you don’t have fragmented care. It’s a really cooperative environment and I think that’s a really important thing, not only for patient experience but also for patient outcomes,” says Dr. Fitzgerald.
“We offer a lot of clinical trials, which offer new treatment options, and we’re about having options and providing people with the information they need to make decisions in a really, really challenging time.”