Inflammatory bowel disease (IBD) is a general term to describe conditions that cause chronic inflammation of the gastrointestinal (GI) tract. Crohn’s disease and ulcerative colitis are the most common types of IBD. An estimated 3.1 million adults in the United States have been diagnosed with a form of IBD, and while most receive the diagnosis as young adults in their 20s or 30s, some adults are newly diagnosed decades later.
Does IBD increase my risk for colorectal cancer?
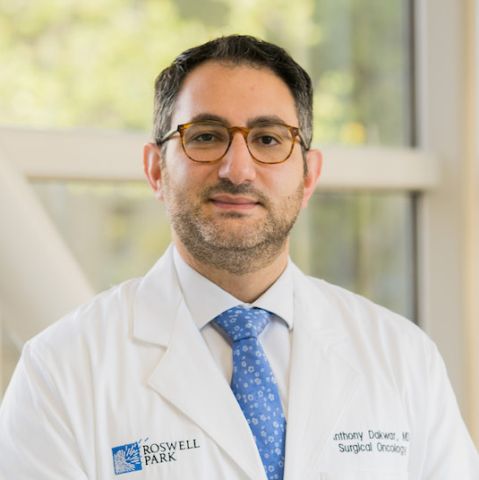
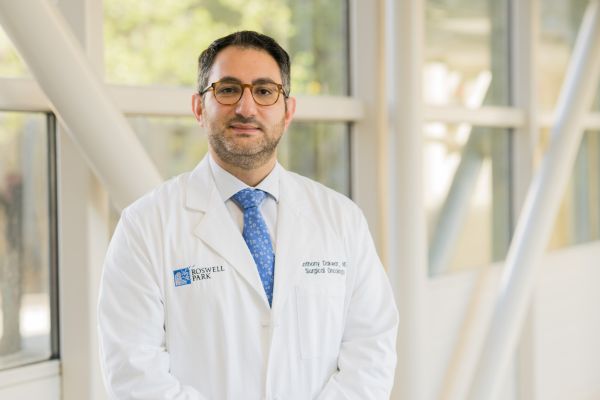
Yes, it does. “Having IBD increases the risk of developing colorectal cancer, due to the effects of chronic intestinal inflammation,” says Roswell Park Comprehensvie Cancer Center colon and rectal surgeon Anthony Dakwar, MD. “Prolonged inflammation of the colon can cause continuous turnover of cells in the intestinal lining, which can lead to tumors formed by rapid and uncontrolled cell growth.”
While the majority of patients with Crohn’s disease and ulcerative colitis will not develop colorectal cancer, their risk for colorectal cancer increases the longer they have IBD. People with Crohn’s disease in particular are two to three times more likely to develop colorectal cancer than people without the disease. In addition, the severity of IBD symptoms and a family history of colon or rectal cancer also play a role in your risk.
| Number of years with ulcerative colitis | Increase in risk of colorectal cancer (compared to general population without ulcerative colitis) |
|---|---|
| 10 | 2% |
| 20 | 8% |
| 30 | 18% |
If I have IBD, what can I do to decrease my risk for colorectal cancer?
First and foremost, you should have regular visits with a gastroenterologist to monitor your condition, says Dr. Dakwar. “Your GI doctor can determine how often you should have screening tests (such as colonoscopies), what medicines you should take to help control inflammation caused by IBD, provide advice on nutrition and ways to limit flare-ups and discuss other lifestyle steps to help minimize risks of cancer.”
Earlier, more frequent cancer screening
While the general population is advised to begin colorectal cancer screenings at age 45, patients with IBD are usually advised to begin screening at an earlier age and on a more frequent basis. “Individual cases will vary, but we generally recommend that patients who have had IBD symptoms for eight years or longer get a colonoscopy every one to two years, even if their IBD is well managed or is in remission,” says Dr. Dakwar.
“If you or your GI doctor notice concerning changes in your symptoms or if your colonoscopy results require more in-depth analysis or multidisciplinary care, your doctor may refer you to resources like Roswell Park’s specialized High-Risk Colorectal Cancer program that offers cancer screenings, genetic counseling and testing, surveillance, and preventive options such as chemoprevention or surgery. Patients with IBD or a family history of IBD or colorectal cancer can also contact Roswell Park directly to request a second opinion or a consult in the high-risk colorectal cancer program,” says Dr. Dakwar.
“Regardless of whether you have IBD, regular screenings, such as colonoscopies, are one of the most powerful and effective tools we have for detecting precancerous and cancerous colorectal conditions.”
Know Your Risk
Complete the Cancer Screening and Prevention questionnaire to understand and manage your risk of colorectal cancer.
Take a Personal Assessment NowEmbrace healthy lifestyle changes
Other steps that can decrease colorectal cancer risk, regardless of whether you have IBD, include:
- Quit smoking
- Exercise regularly
- Eat a high-fiber diet low in fat and red meat
- Limit alcohol intake
- Maintain a healthy weight
Know your health history
Be sure to tell your doctor if you have any of the following risk factors:
- History of colorectal polyps
- Family history of colon cancer, especially among first-degree relatives (parents, siblings or children)
- Certain inherited conditions, such as Lynch syndrome, familial adenomatous polyposis (FAP), or MYH-associated polyposis
- Personal history of colorectal cancer or cancer of the ovaries, uterus, breast or genitourinary tract
"Genetic factors are related to some cases of both IBD and colon cancer, so it is important to tell your doctor about any family history of any of the conditions or diseases noted above. If you have any of these conditions, you would also be a good candidate for a high-risk colorectal cancer screening program like the one offered at Roswell Park,” says Dr. Dakwar.
Is cancer treatment different for patients with IBD?
“At Roswell Park, treatment for all of our patients is individualized, based on factors including the patient’s general health, the stage and grade of the cancer and any genetic mutations that be a factor,” says Dr. Dakwar.
“In some cases a patient with IBD-related colorectal cancer may indeed have the exact same treatment as a patient whose colorectal cancer is not caused IBD, and in some cases they will not.”
“Researchers around the world are studying the role of genetics, diet, immunotherapy and new types of drugs to decrease and prevent IBD inflammation,” says Dr. Dakwar. “But the most positive news is that, even while the incidence of colorectal cancer is increasing for people with and without IBD, the survival rate has improved to 90%, due to earlier and more widespread screening, helping to detect precancerous conditions and cancer at earlier stages, when it is more easily treated.”