Ray Banaszak came to Roswell Park Comprehensive Cancer Center in August 2012 with a plasmacytoma, a cancer of the plasma cells that soon developed into multiple myeloma.
Like many patients, he began a regimen of chemotherapy. “They threw everything but the kitchen sink at me,” Banaszak recalls. In a year and a half, not much had improved, and worst of all, he had to deal with the difficult side effects of treatment.
In February 2014, the Roswell team decided to give Banaszak a series of two in-hospital, 96-hour chemotherapy drips, which dropped the cancer levels down low enough for the team to collect his stem cells to prepare for a transplant.
That June, Banaszak received an autologous stem cell transplant, followed by another three years of chemotherapy treatment with Revlimid (lenalidomide). With his myeloma listed as “in remission” in 2018, he rang the Victory Bell to celebrate.
While in remission, Banaszak took a drug called Darzalex (daratumumab), a targeted therapy aimed at keeping myeloma cells from reappearing. However, prior to having an operation on his Achilles tendon in September 2019, he paused his treatments because they would cause immunosuppression, a slower immune system response that would cause slower recovery from surgery. After the procedure, he resumed treatment, but his care team found out that his body was no longer responding to the drug. That’s when the cancer came back.
New Plan of Attack
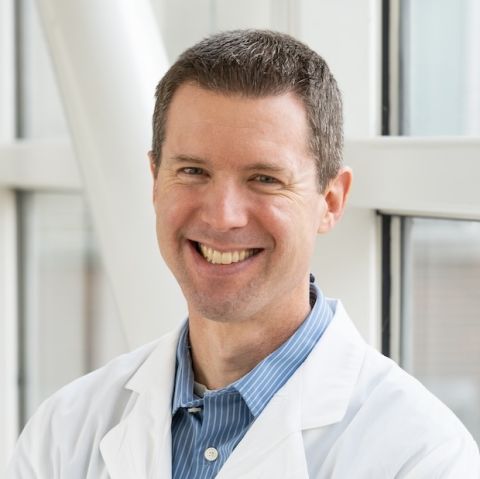
With an already lengthy battle with multiple myeloma behind him, Banaszak needed a new attack plan. “A lot of options had been exhausted with Ray’s prior treatments,” says Jens Hillengass, MD, PhD, Chief of Myeloma at Roswell Park. “Multiple myeloma is tricky because technically, it’s incurable. We didn’t want to close off any future treatment options when figuring out how best to handle things this time around.”
Hillengass estimates that 30-40% of his patients are eligible for clinical trials. For multiple myeloma, new treatments target the B-cell maturation antigen (BCMA) found on the surface of multiple myeloma cells. These treatments are offered through clinical trials and an expanded access program.
“Ray was an outstanding candidate because he had done his homework,” Hillengass says. “He knew a lot about his disease. He read up and was well informed of his options.”
In January 2020, Banaszak enrolled in a study that specifically focused on BCMA using an antibody-drug conjugate known as Belantamab Mafodotin. The study was an expanded access program, which is sometimes referred to as compassionate use. That means the study uses an experimental drug outside of clinical trials. In this case, the FDA granted the drug accelerated approval.
Banaszak received infusions every three weeks. But after the first round, testing showed his disease was unchanged. Nothing happened after the second round of treatment, either. The drug was unsuccessful in pushing the myeloma back into remission.
“I thought it would work,” says Banaszak. “I was disappointed it didn’t, but what did I lose outside of two months? I was happy to try it. Thought it might be my ‘silver bullet.’ If not, the doctors and researchers are going to learn, and it will help them with the next person.
“Having cancer really brings out the fight in you. People with cancer always say, ‘Why me?’ I thought, Why not me?
“My wife worries enough for both of us. I feel that if you worry about things you can’t control, you’re just wasting energy. I am strong enough to deal with this.”
Banaszak’s positive attitude was not lost on Dr. Hillengass, who says, “I knew this wouldn’t stop him from fighting. He wants to live life to the fullest.”
Banaszak adds, “I can change what I can, accept what I cannot and learn from everything else.”
Becoming a Patient Advocate
When Banaszak returned to a traditional chemotherapy treatment used to treat myeloma, an exciting opportunity presented itself. Another patient of Dr. Hillengass was considering a clinical trial. The physician asked Banaszak if he would explain the clinical trial process to the patient, even though his personal experience had not been a success.
“Ray was a perfect choice to explain this process to someone else,” says Dr. Hillengass. “He’s incredibly nice, and he was always so well-informed. This really fits his character. He’s been through so much with his treatments and setbacks, and I knew he would be the best one to help someone else make the right decision for their care.”
“I told the person everything I had gone through and explained some of the things I was concerned about,” says Banaszak. “I let them know it was a positive experience, even though it didn’t work for me. I want to be able to help other cancer patients by explaining what I went through, good or bad, regarding treatments.
“I was given an opportunity by first participating in this study and using that knowledge to help someone decide if they should do it for themselves. I deal with cancer daily by these four things: faith, the support of family and friends, positivity and keeping my sense of humor.”
Multiple Myeloma Clinical Trials
Find out more about the different clinical trials and research studies used to treat multiple myeloma at Roswell Park.
Learn MoreRemission Accomplished
Thanks to his new chemotherapy regimen, Banaszak got some good news in August 2020, when his myeloma went back into remission.
And even with an “unsuccessful” research study in his rearview mirror, he may still benefit from it. “Even though Ray’s results weren’t what we hoped for, this opens the door for a new line of treatment,” says Dr. Hillengass. “Thanks to completing his last study, he is now eligible for another one if he needs it.”
“Cancer patients have to be warriors all the time, but I don’t consider myself one,” adds Banaszak. “I had a lot of help from everyone at Roswell — the positivity from everyone at the front desk, the nurses and everyone I met. Everyone is dedicating their careers to helping others. Their attitude is contagious. They just told me, ‘We’re going to do everything we can to help you.’”
Dr. Hillengass gives him a lot more credit than that. “He’s an impressive person, going through his disappointments with such a great attitude. He’s such a kind person. He brings so much positivity. I can count on him to wear these funny T-shirts at the clinic and make everyone laugh. It’s great to see him doing well.”
Editor’s Note: Cancer patient outcomes and experiences may vary, even for those with the same type of cancer. An individual patient’s story should not be used as a prediction of how another patient will respond to treatment. Roswell Park is transparent about the survival rates of our patients as compared to national standards, and provides this information, when available, within the cancer type sections of this website.