Eunice Wang, MD, Chief of the Leukemia Service at Roswell Park, talks about the difference between acute and chronic leukemia, and describes how quickly they develop and progress.
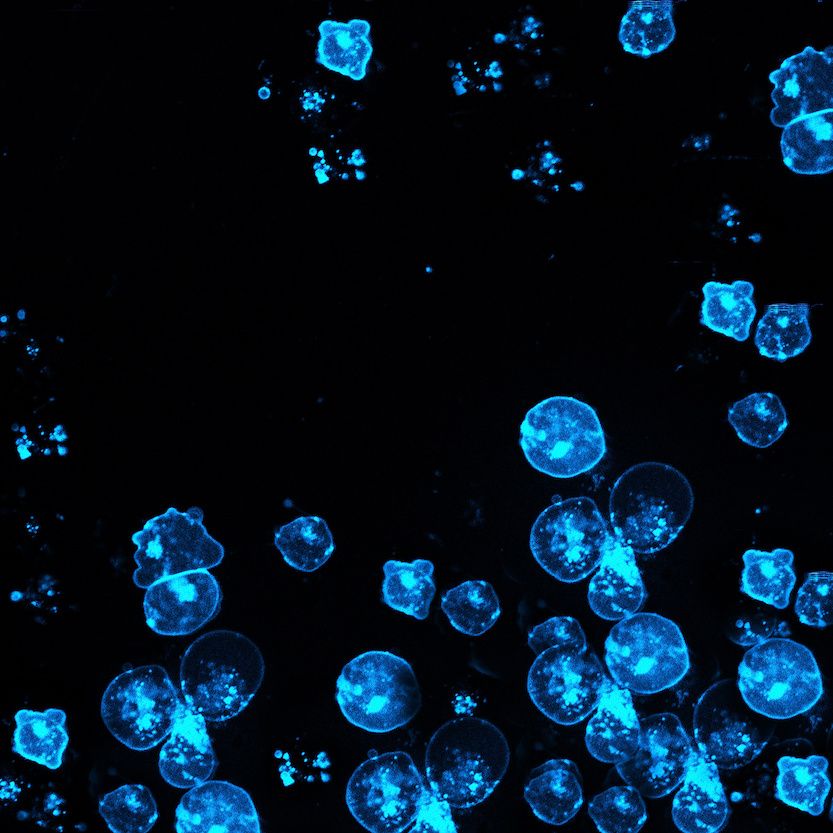
Leukemia is a cancer of the blood. It begins when the bone marrow starts to rapidly produce abnormal white blood cells called leukemia cells. They may crowd out normal white blood cells, red blood cells, and platelets, making it hard for the normal cells to do their work.
There are four main types of leukemia:
- Acute lymphocytic leukemia
- Chronic lymphocytic leukemia
- Acute myeloid leukemia
- Chronic myeloid leukemia
Chronic and acute leukemias are completely different diseases, and they progress at different speeds. The way they’re treated can be very different.
Adult Leukemia & Other Blood Disorders
Leukemia is the name given to several types of cancer that begin in the tissue that creates blood cells. To understand leukemia, it helps to know how normal blood cells form.
Learn MoreAcute leukemia: The most rapidly progressing cancer we know of
Acute leukemias — which are incredibly rare — are the most rapidly progressing cancer we know of. The white cells in the blood grow very quickly, over a matter of days to weeks. Sometimes a patient with acute leukemia has no symptoms or has normal blood work even a few weeks or months before the diagnosis. The change can be quite dramatic.
Extreme fatigue is usually the first symptom that causes acute leukemia patients to seek medical care. They’re tired for no apparent reason. They can’t move and they’re not able to walk, and it comes on fairly quickly. When we check their blood count, their red blood cell count might be half of what’s normal. That’s why they’re exhausted — because they’re not getting enough oxygen.
It’s also common for these patients to develop pneumonia or some sort of infection. They don’t get better after taking antibiotics, so they take more and more, but they still don’t get better. Then finally someone checks their blood count and discovers that they’re not responding because their immune system is very low because of the acute leukemia.
Effects of too many white blood cells
At the time of diagnosis, patients can have very, very high white blood cell counts. Typically a healthy person has a white blood cell count of about 4,000-11,000. Patients with acute or even chronic leukemia may come in with a white blood cell count up into the 100,000-400,000 range.
When you have that many white cells in your blood vessels, it can impair blood flow, because you have 20 to 40 times the normal number of cells in the blood vessels. And these are not normal cells — they are tumor cells, so they can stick together, and they can also stick to the blood vessels.
When patients have very high white blood cell counts, the leukemia cells will usually spill over from the blood vessels into some of the organs. If the lungs are affected, the patient can have respiratory failure. Patients can have strokes because of interrupted blood flow in the brain. They can have heart attacks or neurological changes. So when someone comes in with a very high white blood cell count, we are very concerned about these risks. In those cases, we usually try to quickly remove the abnormal cells from the blood and start chemotherapy to begin killing them off as soon as possible.
Leukemia can also cause the body to make fewer platelets, which help the blood to clot. When that happens, patients have a higher risk of bleeding, so they may wind up in the emergency room or urgent care center after developing a nose bleed that lasts for two hours. So if you have abnormal bleeding from a small injury or you wake up with enormous bruises and don’t remember having injured yourself, that could mean that something is wrong with your platelets and your clotting system.
Low platelets can also cause petechiae, little breaks in the smallest blood vessels that cause blood to leak into the skin. Petechiae cause dark-red spots to appear on the skin, looking very much like a rash.
Request an appointment
Make an appointment by calling 1-800-ROSWELL (1-800-767-9355).
Request an appointmentChronic leukemia may go undetected
Unlike acute leukemia, chronic leukemia develops slowly. It may take months or even several years before the disease begins to cause symptoms that alert the patient that something is wrong.
Because chronic leukemia is very slow-growing and may not cause symptoms, it’s common for the disease to first be detected in normal blood work when a patient goes to the doctor for a regular checkup. If a patient doesn’t see a doctor for several years, the disease can go undetected over a long period of time, and the abnormal cells can build up and cause an enlarged spleen.
Why we don't stage most leukemias
With solid tumors, at the time of diagnosis, we usually say that the cancer is stage I, II, III, or IV, based on how far away the cancer cells have spread from where they began. If you have breast cancer and the cancer is located just in your breast, that is stage I. If it has traveled far from the breast, into the brain or liver, we would consider that stage IV.
But leukemias are in the blood, so at the time of diagnosis, the leukemia cells are already in your blood and bone marrow. They are already throughout the whole body. That’s why we don’t stage most of the leukemias as we do with solid tumors. Instead, we say that either you have active disease or the disease is in remission.
The only exception to that is chronic lymphocytic leukemia, or CLL, which acts a little bit more like a lymphoma and can spread throughout the body through lymph, blood, or bone marrow and lymph nodes throughout the body. For that particular type of chronic leukemia, we do say there are stages.
We have time to develop the best treatment plan
We were always taught that acute leukemia is an emergency and that we need to start therapy right away. That is still true for some patients. The urgency is to manage any life-threatening complications, such as those mentioned earlier — for example, stroke or respiratory failure.
However, over the last few years, several drugs have been approved for acute leukemias that focus on destroying cells that have specific mutations. We know there are patients who won’t benefit from chemotherapy but who might benefit from these types of targeted approaches. So now the recommendation is that if a patient with acute leukemia does not have a life-threatening complication, you may be able to wait a few days to get additional information about the disease that can help identify the best treatments.
At Roswell Park we still keep an eye on those patients, either in the inpatient center or with very close monitoring while they are at home. We still want to start treatment as soon as possible, but with most patients, we don’t need to do that within an hour or two after they come to us. We have time to complete testing that will help us design the best therapy.
Chronic leukemias can be controlled or treated in much the same way as other chronic disorders, such as high blood pressure. Patients may just be monitored with blood work and physical exams over a period of months to years before they need treatment.