Polyps are most likely to develop in menopausal or postmenopausal women
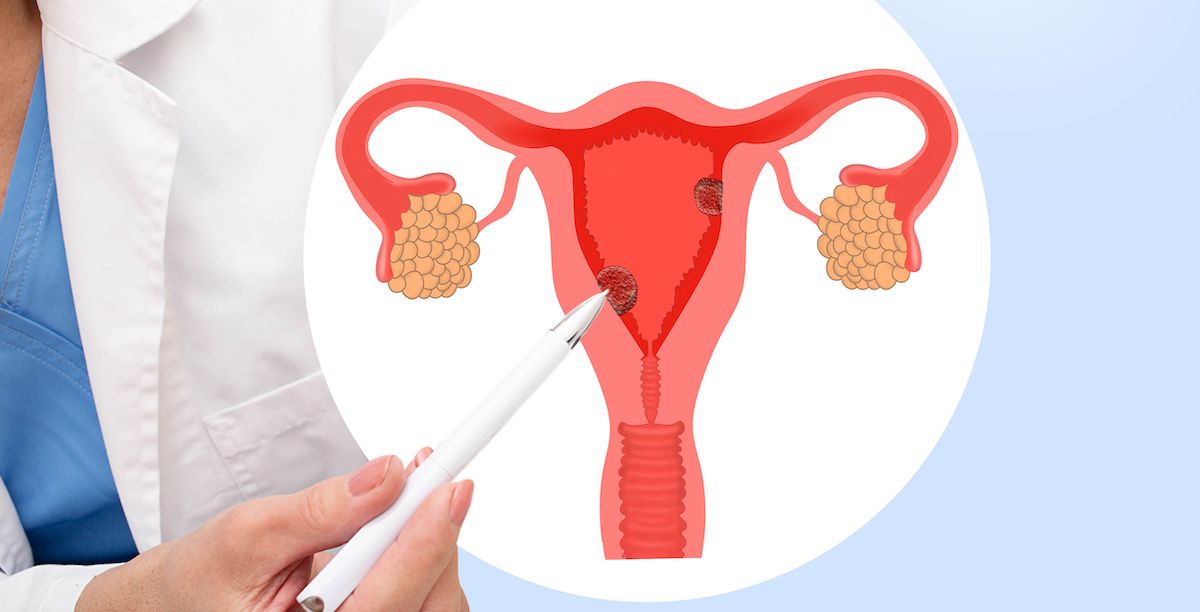
Uterine polyps are growths that form in the inner lining of your uterus, called the endometrium. They may form as one or many, are round or oval in shape, range from the size of a sesame seed to the size of a golf ball or larger, and attach to your uterine wall by a large base or thin stalk.
Also known as endometrial polyps, they are the result of overgrowing cells in the uterine lining and are generally found in women who are going through or have completed menopause.
“Uterine polyps are usually benign, or noncancerous, but may cause problems with menstruation or fertility if left untreated,” explains Peter Frederick, MD, Chief of Gynecologic Oncology at Roswell Park Comprehensive Cancer Center.
The chances of a uterine polyp turning into cancer are about 1-2 percent in premenopausal women, and 5-6 percent in women who have gone through menopause. They are rarely found in people under 20 years old.
What causes uterine polyps?
While there is no single determinant of polyps, age is a major predictor. You are most likely to develop them in your 40s or 50s, if you are going through or have gone through menopause. While researchers don’t know exactly why polyps form, they believe hormone levels may be a factor. Estrogen causes the endometrium to thicken during the menstrual cycle, which likely contributes to uterine polyp growth, and known risk factors for uterine polyps involve exposure to high amounts of estrogen.
What are symptoms of uterine polyps?
Uterine polyps often don’t have symptoms. For this reason, many women are never diagnosed. The most common symptom is abnormal bleeding, which may include:
- Vaginal spotting or bleeding after menopause
- Irregular menstrual periods (longer or shorter than usual)
- Unusually heavy bleeding during menstrual periods
- Bleeding or spotting between periods
- Bleeding after intercourse
Infertility, being unable to become pregnant or carry a pregnancy to full term can also be a symptom. And while pain isn’t a common symptom of uterine polyps, large ones sometimes cause dull aching in your abdomen or lower back similar to menstrual cramps.
Sometimes, polyps can also slip through your cervix (the opening between your vagina and your uterus), and may be seen during a physical exam.
How are uterine polyps diagnosed and treated?
If you think you may have symptoms of uterine polyps, your provider will review your medical history and symptoms: any bleeding or spotting if you are post-menopausal, specifics about your menstrual cycle, and whether you’ve had any difficulty getting pregnant.
Your provider may also perform a gynecological exam that includes a pelvic exam. Other tests include:
- Transvaginal ultrasound — to provide an image of the inside of your uterus, including any irregularities.
- Endometrial biopsy — to collect soft tissue from the inner walls of your uterus and test it in the laboratory for any abnormal cells.
- Curettage — to scrape tissue from any existing polyps to determine if cancer cells are present.
“Treatment for uterine polyps depends on your symptoms and your individual risk of uterine cancer. If you are still in your reproductive years, and the polyp isn’t causing symptoms, your provider may decide just to monitor it,” Dr. Frederick says. “You may need treatment if you are post-menopausal, or have symptoms. Treatment may include medications that keep your hormones balanced or the removal of the polyps.”
If the polyp is determined to contain cancer cells, you may need a hysterectomy, which involves the removal of your uterus.
Why Roswell Park for uterine cancer?
Roswell Park Comprehensive Cancer Center offers treatments at the forefront of cancer care, plus clinicians with the knowledge and experience to use them. Treatment for uterine cancers may include:
- High-volume surgical experience in laparoscopic, robot-assisted and complex gynecologic surgery, including radical debulking surgery that’s essential for regional chemotherapy.
- Personalized medicine based on advanced genomic testing.
- Clinical trials to access the very latest drugs, immunotherapies and targeted agents — oftentimes years before they become available from other providers.
- Oncofertility Program provides information about how fertility and intimacy may be affected by uterine cancer treatment and options for fertility preservation.
“Although uterine polyps cannot be prevented, they are generally not harmful. Regular checkups with your gynecologist allow your provider to detect them early so they don’t lead to complications or unpleasant symptoms,” Dr. Frederick advises.
If you are experiencing symptoms, research shows that removal eases symptoms in 75% to 100% of cases. Uterine polyps rarely grow back after they are removed. If they do, your provider will be able to recommend additional treatments.