September is Sickle Cell Awareness Month, bringing attention to a common but seldom discussed blood disorder that has a large impact on the Black community — one in 13 people of African descent, including people from Haiti, carry a genetic trait for sickle cell. One in 100 people of Hispanic/Latinx descent carry carry a sickle cell trait, and it also is found in people of Southern Mediterranean, Middle Eastern, and Indian/South Asian descent. Having sickle cell trait puts you at risk for having a child with sickle cell disease.
Carrying the genetic trait (in DNA) for sickle cell, as well as other blood diseases like thalassemia, is most common in people from areas of the world where the risk of malaria is high.
“Having a trait for one of these diseases makes you more likely to survive a malarial infection, meaning there will be more people with these traits in those areas,” says Steven Ambrusko, MD, MS, a pediatric hematologist/oncologist at Roswell Park Oishei Children’s Cancer and Blood Disorders Program, and Director of the Sickle Cell & Hemoglobinopathy Center of Western New York.
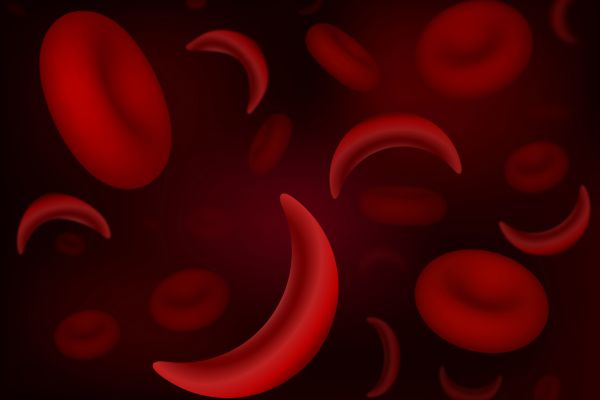
Sickle cell disease is characterized by blood cells that become oddly shaped due to abnormal hemoglobin, turning the normally donut-shaped cells into crescent, or sickle-shaped cells. These abnormal cells can damage and then block the small blood vessels of the body, causing pain and potential tissue damage. It can be compared to the pins-and-needles feeling that happens when you sleep on your arm, but these “pain crises” are usually many times worse and not quickly resolved. The abnormal sickle cells also break apart more easily, which causes anemia (low number of red blood cells).
Screening tests for sickle cell disease and thalassemia, a related blood disease in which a person doesn’t make enough of the protein for hemoglobin causing various levels of anemia, are performed in newborns, Dr. Ambrusko says. Being diagnosed with sickle cell disease also increases a person’s risk for severe infections especially in young children, blockage of sickle cells in the lungs causing a mild to severe condition called acute chest syndrome, and can lead to strokes in children as young as 2 years of age.
A recessive gene trait
There are several kinds of sickle cell disease, each of which depends on which sickle cell trait children inherit from their parents. Because the traits are recessive, a child born with sickle cell disease would receive them on genetic material from both parents, Dr. Ambrusko says.
“The most common kind of sickle cell disease from inheriting a copy of the sickle cell gene from each parent (called ‘SS-type’), is the most severe but there is a lot of variability. It’s also a progressive disease; it tends to get worse as you get older. There are some people who have a mild case and it stays mild; there are people who start off with a mild case and get worse, and you can have people who start off bad from the get-go and get worse.”
Dr. Ambrusko stresses the importance of staying well hydrated and eating a healthy diet high in the antioxidants found in fruits and vegetables and low in processed foods. It’s also important for people with sickle cell disease to avoid pain triggers, like exposure to cold temperatures, and to treat their pain aggressively and immediately to avoid acute worsening of pain, as well as long-term bone and tissue damage. Many people with sickle cell disease are candidates for treating their disease with hydroxyurea, which helps decrease or even prevent the formation of sickle-shaped red blood cells. Others with more severe disease may benefit from receiving regular blood transfusions to keep most of their blood “normal” to decrease the risk of severe complications like stroke.
For patients who have severe cases of sickle cell disease, Dr. Ambrusko often recommends a bone marrow transplant, the only established cure for sickle cell disease. While bone marrow transplantation is a procedure with significant risks, sometimes those risks are much less than the progressive and potentially life-threatening risks of the sickle cell disease itself.
Know your status
It’s important for potential parents to know and understand their sickle cell status and to talk with their spouse or partner about the recessive sickle cell trait or related traits they may carry.
“People with abnormal hemoglobin traits have risks of having children with a potential blood problem, including the risk of sickle cell disease,” Dr. Ambrusko says. “A child might have another form of sickle cell disease, like sickle thalassemia, a combination of both sickle cell and thalassemia. But these are not part of routine blood tests, and would not be found in a simple blood count. A special type of test for types of hemoglobin called a hemoglobin electrophoresis is needed to know whether a person carries these traits.”
Dr. Ambrusko says while his work as a pediatric hematologist is with children, he will see in consultation adults with sickle cell disease if they need help.
“If there are adults who feel they have not been getting appropriate care or want help for better disease management, I am happy to see them to provide some guidance and recommendations,” he says.