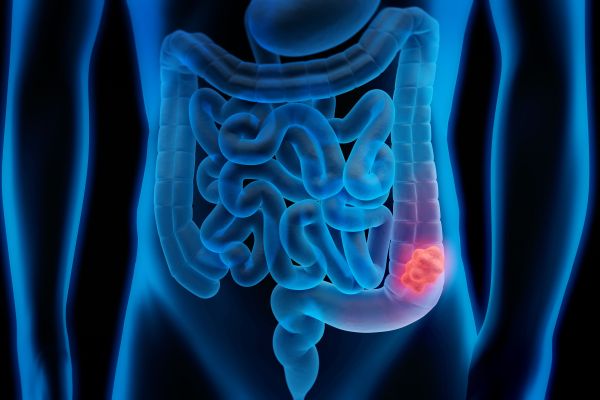
If a polyp is found early, doctors can remove it and stop colorectal cancer before it starts.
What is a polyp?
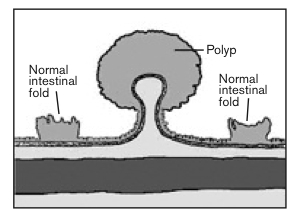
A polyp is an abnormal growth on the inner surface of the large intestine, which includes the colon and the rectum. It's possible to have multiple polyps that are flat or raised (as if they are on a stalk). Polyps are one of the most common colorectal conditions, occurring in 15 - 20 percent of the adult population. They can occur anywhere in the large intestine or rectum, but are more commonly found in the left colon, sigmoid colon, or rectum.
Some colon polyps are benign, which means they are not cancerous, but some can be precancerous or cancerous. The relationship of certain polyps to cancer is well established. Polyps can usually be removed during colonoscopy.
What are the risk factors?
Anyone can get colon polyps, but certain people are more likely than others to get them. You may have a greater chance of getting polyps if:
- You are 45 years of age or older
- You have had polyps before
- Someone in your family has had polyps
- Someone in your family has had colon or rectal cancer
- You have had uterine or ovarian cancer before age 50
- You use tobacco products (smoking, chewing tobacco, etc.)
- You drink alcohol
- You don’t exercise
- You are overweight
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!What are the symptoms?
Most people with colon polyps do not have symptoms. Often a doctor finds them during a regular checkup or while testing for something else.
Some people do have symptoms, such as:
- Bleeding from the anus (you might notice blood on your underwear or on toilet paper after you’ve had a bowel movement.)
- Change in bowel habits (constipation or diarrhea that lasts more than a week)
- Blood in the stool (may look like red streaks or make the stool black)
- Mucus drainage from the anus If you have any of these symptoms, see your doctor.
How are polyps diagnosed?
Polyps are diagnosed by either looking at the colon lining directly (colonoscopy) or by a specialized CT scan called CT colography (also called a virtual colonoscopy). Barium enema x-rays have been used in the past and may be appropriate in some circumstances.
- Endoscopy: There are three types of colorectal endoscopy: rigid sigmoidoscopy, flexible sigmoidoscopy, and colonoscopy. Rigid sigmoidoscopy permits examination of the lower 6 – 8 inches of the rectum. In flexible sigmoidoscopy, the lower 1/4 - 1/3 of the colon is examined. Neither rigid nor flexible sigmoidoscopy requires medication, and both can be done in the office. Colonoscopy uses a longer, flexible instrument and usually allows inspection of the entire colon. Bowel preparation is required, and sedation is often used. Both sigmoidoscopy and colonoscopy allow the removal of polyps.
- Computerized tomography (CT) colonography: With this test, also called virtual colonoscopy, the doctor puts a thin, flexible tube into your rectum and inflates it with air. X-rays are taken and computers create pictures of the large intestine that can be seen on a screen. The CT scan takes less time than a colonoscopy because polyps are not removed during the test. However, this test still requires a bowel preparation to clean out the colon. If the CT scan shows polyps, you will need to have a colonoscopy so the polyps can be removed.
- Barium Enema: The colon can be examined indirectly using the barium enema x-ray technique. This examination uses a barium solution that is put into the colon through the anus to coat the colon lining. X-rays are taken. The colon looks white from the barium, and polyps appear dark. This test is not used as often now as in the past.
- Stool test: The stool is tested in the laboratory for signs of cancer, such as DNA changes or blood. Although checking the stool for microscopic blood is an important test for colon and rectal disorders, a negative test does NOT rule out the presence of polyps.
Who should get tested for colon polyps?
Talk with your doctor about getting tested if you are 45 or older. You may start screening tests at a younger age if you have symptoms or if someone in your family has had polyps or colon cancer.
Do polyps need to be treated?
Since there is no foolproof way of predicting whether or not a polyp is or will become cancerous, total removal of all polyps is advised. The vast majority of polyps can be removed by snaring them with a wire loop passed through the instrument. Small polyps can be destroyed simply by touching them with a coagulating electrical current. Most colon exams using the flexible colonoscope, including polyp removal, can be done on an outpatient basis with minimal discomfort. Large or flat polyps may require more advanced resection techniques. These include:
- Endoscopic Mucosal Resection: A technique used to remove cancerous or other abnormal lesions found in the digestive tract.
- Endoscopic submucosal dissection: An advanced endoscopic procedure used to remove gastrointestinal tumors that have not entered the muscle layer.
How can I prevent colon polyps?
Doctors do not know of any sure way to prevent polyps, but you may be able to lower your risk by making healthier choices and changing poor habits.
- Eat more fruits and vegetables and less fatty food
- Don’t smoke
- Avoid alcohol
- Exercise most days of the week
- If you’re overweight, lose weight
- Eat more foods with calcium (milk, cheese, yogurt, and broccoli)
Can polyps come back?
If a polyp is removed completely, it is unusual for it to return in the same place. The same factors that caused it to grow in the first place, however, could cause polyp growth at another location in the colon or rectum. New polyps will develop in at least 30 percent of people who have previously had polyps.