Sepsis is your immune system’s overwhelming response to an infection. It can progress rapidly, and it is an emergency. Doctors can’t predict who will develop sepsis, but it is most commonly associated with bacterial infections of the lungs, kidney, bladder, GI tract, skin and blood. It can occur with fungal or viral infections as well, including COVID-19 and the flu. It is more common in people who are — or have recently been — in the hospital, but it also strikes people who don’t even know they have an infection. It’s a leading cause of readmission to the hospital, and of death.
Before antibiotics, even a small scratch could become infected and progress to sepsis, septic shock and death. Today it can still be very difficult to treat some infections due to disease-causing microorganisms (pathogens) that are resistant to the drugs that are used to cure them.
How Do You Get Sepsis?
Anyone can get an infection, and almost any infection can lead to sepsis. More than 1.5 million adults in the U.S. get sepsis every year, and more than 250,000 die from it. The number of cases in the U.S. is on the rise as more people are surviving serious illness and living with chronic illness. Transplants — which require anti-rejection drugs that weaken the immune system — are more common, and bacterial resistance to antibiotics is growing.
What causes sepsis? When a pathogen enters the body in sufficient amounts, your body’s immune system goes into action. White blood cells, chemicals, antibodies, interferon and other substances are released to fight the invader. You may experience symptoms such as fever and inflammation as part of this immune response. (Symptoms may also be caused by the pathogen itself. For example, some bacteria produce toxins that cause symptoms/illness.)
Pathogens can travel through the bloodstream and cause a body-wide infection, or a local infection can become quite severe. Overwhelming infection can send the immune response into overdrive and set off a chain of events that disrupts the circulatory system. Blood may leak from blood vessels, blood clots may form and blood pressures can change. Poor blood flow starves tissues and organs of the oxygen and nutrients they need to live. Severe sepsis can lead to septic shock, with dangerous drops in blood pressure, a weakened heart, multiple organ failure and death.
Who Gets Sepsis?
You may have a higher risk if you:
- Are over age 65 or under one year of age
- Have a chronic medical condition (cancer, diabetes, or lung, liver or kidney disease)
- Have had an organ transplant or are taking medications that suppress your immune system
- Have a weakened immune system
- Have had a serious injury
- Have survived sepsis in the past
The Three Stages: Sepsis, Severe Sepsis, Septic Shock
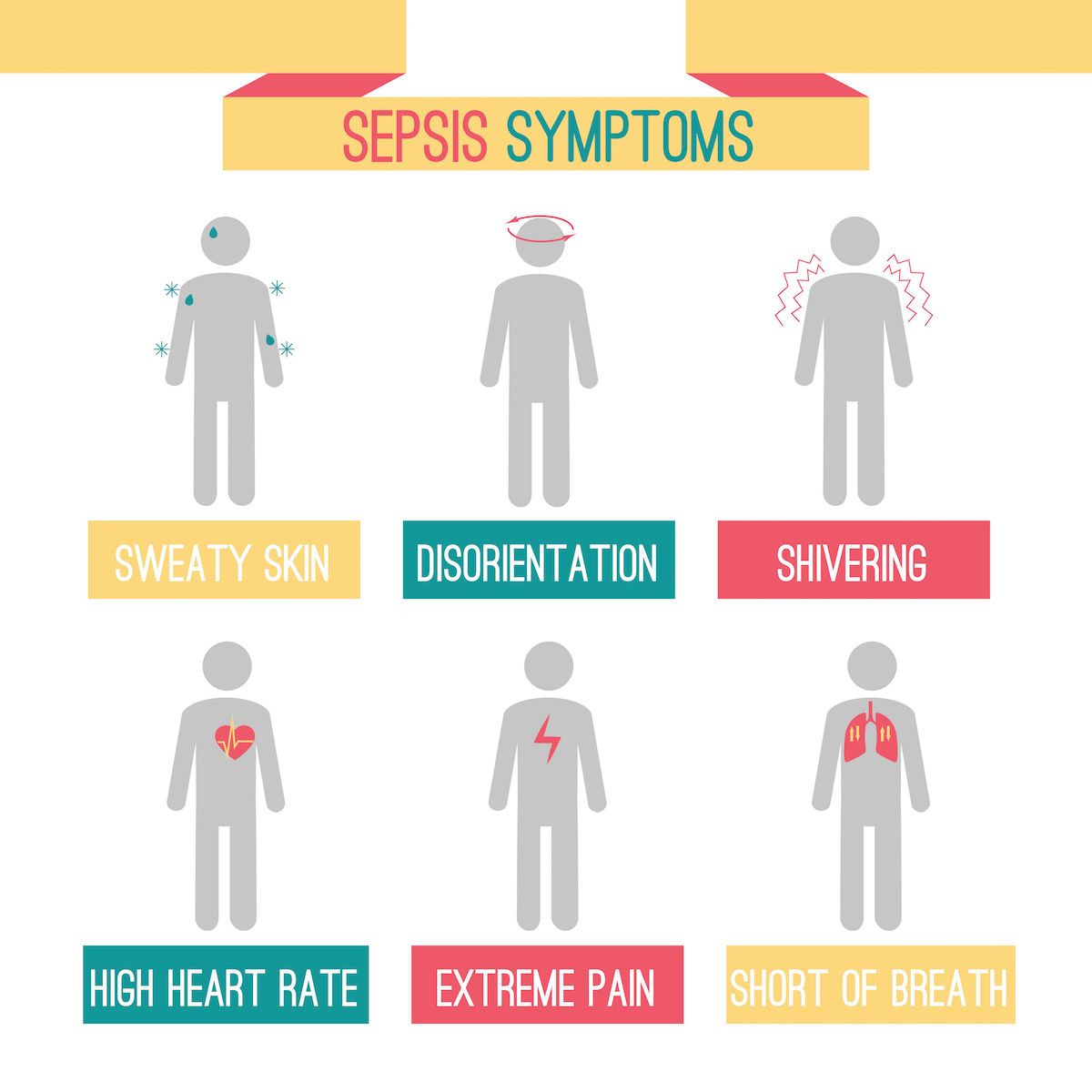
It can be difficult to diagnose sepsis, especially in the early stages. Symptoms may be vague or similar to other illnesses. Blood cultures may fail to identify the pathogen causing the infection, making it difficult to know what medication would be most effective. Symptoms can vary from person to person.
If you develop symptoms of sepsis, seek medical care immediately.
- Fever over 101°F/38.4°C or low body temperature (below 96.8°F/36°C). Chills, shivering due to changes in body temperature
- Rapid breathing — over 20 breaths/minute
- Fast heart rate — over 90 beats/minute
- Shortness of breath
- Low blood pressure
- Anxiety/feelings of doom
- Low platelet count (increased risk of bleeding/hemorrhaging)
- Mental/cognitive changes
- Decreased urination
- Trouble breathing
- Abnormal heart functions
- Extreme discomfort or pain
- Skin appears mottled
- Extreme weakness
Symptoms of septic shock are the same as those of severe sepsis, but there is also an extreme drop in blood pressure. Shock is diagnosed when replacement fluids are given but they fail to bring blood pressure back up, and major organs start to fail because they are not getting the blood supply they need.
How Is Sepsis Diagnosed?
- Presence of an infection is suspected or confirmed
- Physical exam
- Review of medical history and present symptoms
- Blood tests to check white blood count (which rises with infection) and identify the pathogen
- Imaging study (X-ray, CT scan) to locate areas of infection
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!How Is Sepsis Treated?
If you have sepsis and aren’t already in the hospital, you will probably be admitted and may wind up in the intensive care unit. Your doctors will try to identify and treat the infection (antibiotics for a bacterial infection) and give medications and fluids to prevent a drop in blood pressure and maintain circulation to your organs. If organs start to fail, you may need help to maintain basic functions — for example, with dialysis or a ventilator.
Afterward
Many people survive sepsis and return to their normal life. If they had a chronic illness before getting sepsis, they are more likely to have permanent damage to an organ. The immune system may also be permanently affected by a bout of sepsis, which can cause problems if you get sick in the future. The Global Sepsis Alliance reports that many survivors suffer lifelong aftereffects, such as sadness, anxiety, swallowing problems, sleeping problems, memory/thinking/concentrating problems, fatigue and muscle weakness.
For More Information
Centers for Disease Control
Journal of the American Medical Association – Patient Page