“Within five years, cancer will have been removed from the list of fatal maladies.” That was the optimistic promise to U.S. President William Howard Taft in 1910 when he visited Buffalo’s Gratwick Laboratory, now Roswell Park Comprehensive Cancer Center. More than a century later, it’s reasonable to ask, “What’s taking so long?”
Here are just a few things we know now that we didn’t know then.
Cancer is not one disease. It’s hundreds of diseases.
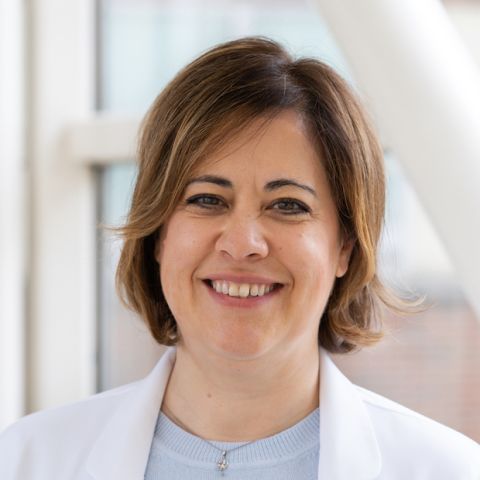
“Cancer is as individual as the person who has it,” explains Joyce Ohm, PhD, Department of Cancer Genetics and Genomics at Roswell Park.
“Let’s say there are identical twin sisters, both with breast cancer. They may have been born with exactly the same genetic mutations, but one responds to therapy and one doesn’t. One may live and one may die.”
How can the outcome be so different for identical twins? Environmental epigenetics may be one reason. Although the twins were born with the same DNA, throughout their lives they were exposed to different influences — for example, pesticides, viral infections, smoking, unhealthy foods or even traumatic experiences — that could have switched normal genes on or off, such as the tumor-suppressor genes responsible for shutting down cancer cells when they begin to grow. That could affect the twins' individual risk for developing cancer.
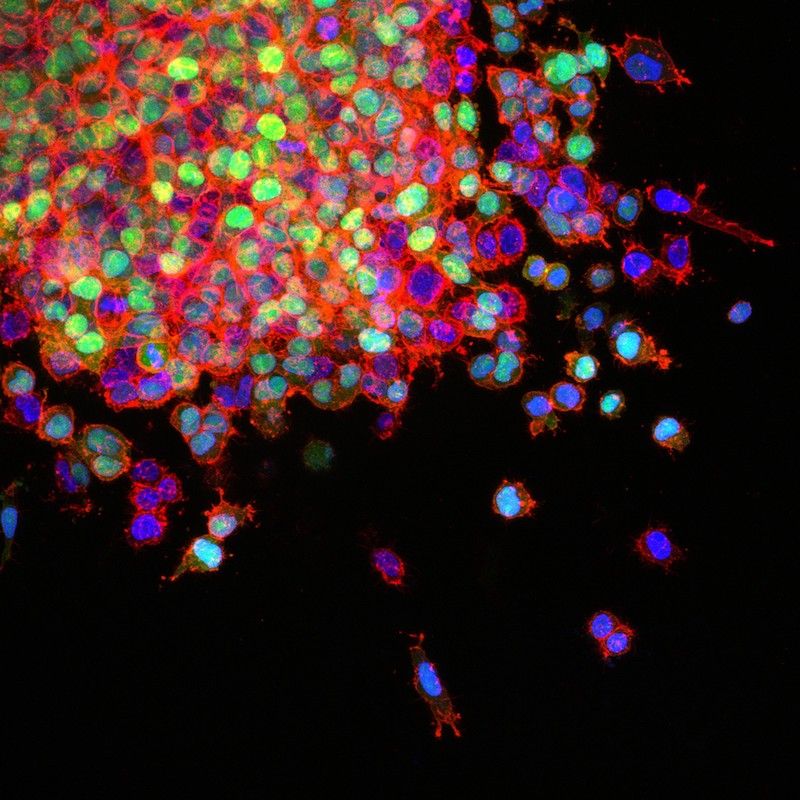
The DNA changes that caused the cancer cells to grow in the first place make the cells multiply too fast and cause them to behave abnormally. “With a cancer cell, it’s as if you let a two-year-old pack for your Disney vacation, but you don’t check what’s in the suitcase,” says Ohm. “You might have a bathing suit, but you might also have a can of green beans. The cells are completely screwed up.”
As the process continues and the cells collect to form a tumor, the DNA changes spin even further out of control until the cells are all very different from one another — and even different from the “mother” cell where they first began.
In a nutshell, the DNA of the tumor ends up being different from the DNA of the patient, and certainly different from the DNA of anyone else’s tumor, including the patient’s identical twin.
Request an Appointment
Make an appointment by calling 1-800-ROSWELL (1-800-767-9355).
Request an AppointmentMany tumors contain more than one type of cancer cell.
This is true for ovarian cancer, renal cell carcinoma, breast cancer, chronic lymphocytic leukemia (CLL) and other cancers. While one type of cell in the tumor may respond to treatment, other types can escape unharmed and continue growing. “Even if 99% of the cells respond, the tumor’s still going to grow back from that 1% that didn’t respond,” says Ohm.
To get around the problem, different types of therapies can be combined to “hit the tumor with all the right things and get rid of it.”
Cancer cells can change over time.
Sometimes a drug works well at first, but later the cancer becomes resistant and continues to grow, because the cancer cells have mutated, or changed genetically. In fact, although normal cells can mutate, cancer cells are 100 times more likely to do that.
The good news is that new therapies are being introduced all the time — including many available through clinical trials — so when the current treatment fails, some patients are able to move on from one new treatment to another. That’s the case for many patients with chronic myeloid leukemia (CML). “Yes, patients have to change therapies, and they’re on therapies for a long time, but their lives can be extended for years and years,” notes Dr. Ohm. “CML is a disease we know how to treat.”
Cancer cells are “super good at staying alive.”
When the body works as it’s supposed to, a cell that becomes abnormal will self-destruct in a process called apoptosis. “But apoptosis gets turned off in a lot of cancer cells,” says Ohm. “Cancer cells are super good at staying alive.”
Cancer cells can also find ways to protect themselves from treatment. Here’s one example: Testosterone, which is manufactured in the testicles, “feeds” prostate cancer, so some prostate cancer patients receive hormone therapy to block the body’s production of testosterone. However, in some cases, the tumor cells then develop the ability to make testosterone from cholesterol.
Will we ever find a cure?
“We’re making progress,” says Dr. Ohm. “It feels slow, and sometimes it’s not fast enough for our patients. We know that, and that’s hard, but we are making tremendous progress.”
The mapping of the human genome in 2003 — a historic international achievement in which Roswell Park played a role — contributed vast amounts of information for solving the puzzle. It has helped researchers identify 291 genes associated with cancer risk and made possible such breakthroughs as genomic analysis, which matches the DNA of the patient and the tumor to the targeted therapies that are likely to work best.
And immunotherapy, once viewed as having limited potential, is showing great promise, especially with the development of new cellular therapies.
“Today, when treatments do fail, we have a bigger toolbox,” says Dr. Ohm. “We have something else we can offer that we didn’t have a short time ago. In the past we would have said, ‘I’m sorry, there’s nothing else we can do.’
“Breast cancer’s a great example. Twenty years ago, the disease would progress in early-stage patients. Now it doesn’t. Now we know how to treat an early-stage patient. Now patients are living who once wouldn’t have lived. The key is increasing the number of patients we can help and making those treatments better.
“The harder ones are the rarer tumors — the ones we haven’t gotten a handle on yet, like pancreatic cancer and small-cell lung cancer and glioblastoma.
“But we beat cancer here every day. Every day patients survive who would not have survived even five years ago. Every day patients are being cured with new advances that are coming along the line. Some patients beat this and we monitor them for a long time, and they don’t ever get it back.
“And for those patients, that’s all that matters.”
Find out how patients, their friends and families are helping speed research through Roswell Park's Data Bank and BioRepository (DBBR).