A cancer diagnosis can trigger a massive wave of anxiety. First comes the most important question: Will I survive? — followed quickly by the second: How am I going to pay for this?
There’s growing evidence that the emotional burden of out-of-pocket medical expenses, sometimes called financial toxicity, can affect people physically and result in poorer survival, especially among cancer patients. Research at Roswell Park Comprehensive Cancer Center is shedding light on why that happens, and a new financial navigation program for patients is helping turn the tide.
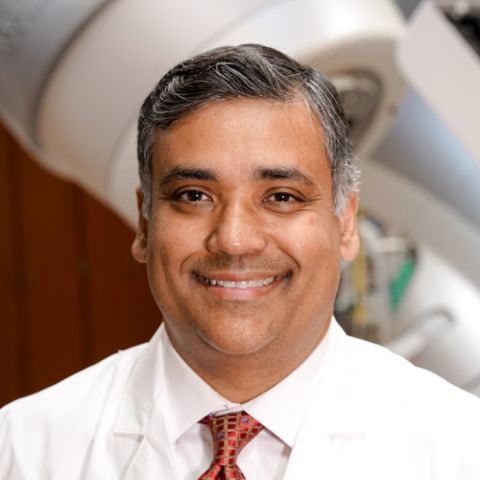
“We’ve been surveying our patients for more than a year to get insights on their quality of life,” says physician Anurag Singh, MD, Director of Head & Neck Radiation Services. “One of the questions we asked was, ‘How worried are you about your finances?’ We found that there was a huge survival difference between patients who said they were somewhat or very worried about their finances compared with those who said they were only a little worried, or not at all.
“We saw that financial toxicity was not only a huge cultural and social problem but also an active therapeutic problem, and we knew we had work to do to address this.”
Financial stress impacts cancer treatment
Picking up from seminal research by Roswell Park immunologist Elizabeth Repasky, PhD, Dr. Singh and colleagues looked at how stress impacts the effectiveness of chemotherapy and radiation therapy. The team discovered that when a patient is worried about money, markers in the blood signal the presence of inflammation, which can help cancers grow and spread. “The markers change when you’re stressed in general,” he explains, “but when you’re worried about money, that’s a huge stress, and it impacts every other aspect of stress.”
There are many ways to relieve financial stress, and Tameka Brooks is well acquainted with them. As a relationship banker for more than a decade, she often provided financial services to patients and their families who faced heavy medical expenses after a cancer diagnosis. “Sometimes they would come to my desk crying,” she says. “They’d say, ‘I don’t know what to do.’”
Her passion for that work led her to Roswell Park, where she was hired as Community Outreach Manager and Financial Empowerment Coach within the Community Outreach and Engagement team. For more than a year she has partnered with the Roswell Park Head & Neck Center, where she provides financial navigation to patients. “Dr. Singh loves his patients and wants them to have good outcomes,” says Brooks. “Together we’re the dynamic duo.”
Working with Dr. Singh and Elizabeth Bouchard, PhD, who heads Roswell Park’s Community Outreach and Engagement program, Brooks developed a financial navigation program, and together they’re evaluating its effectiveness in a randomized, controlled trial at Roswell Park.
Patients can opt to either take home a printed guide or arrange a one-on-one meeting with Brooks for personalized navigation. She starts by asking them to name their three top concerns and helping them develop a budget if they don’t have one already. “Everything is connected to your finances,” she says. “A budget helps you see where your dollars are going. Sometimes it’s as simple as that.”
She makes it clear that financial stress isn’t limited to patients in low-income brackets. “I see people from all different circumstances and cultures who are having trouble. A cancer diagnosis can be so overwhelming that it takes a bit of your pride and your confidence. To overcome that, I meet them right where they are. Whatever they want to discuss, we discuss.”
Finding ways to lift the burden of stress
Brooks has developed relationships with government agencies and community organizations that assist with a wide range of needs, from child care and transportation to food and housing. Sometimes solving a problem is as easy as streamlining: If transportation is expensive and the patient has appointments at Roswell Park on three different days of the week, creative scheduling may reduce that to one or two days.
Because many people are already overwhelmed by their treatment and diagnosis, taking on one more task can seem impossible, so she guides them in looking for grants that provide financial support for cancer patients or joins them on a phone call when they want to check their eligibility for services.
The process works, according to one of the studies Roswell Park conducted with radiation oncologist Mark Farrugia, MD, PhD. “We saw that when our patients didn’t have financial counseling, their financial worries increased during treatment,” notes Dr. Singh. “When they did get financial counseling, they were stable during treatment.” The team hopes the results of their program will provide the basis for expanding financial navigation services for cancer patients.
“This is going to give patients some peace, empowerment and the ability to focus on their health,” says Brooks. “That’s the goal.”