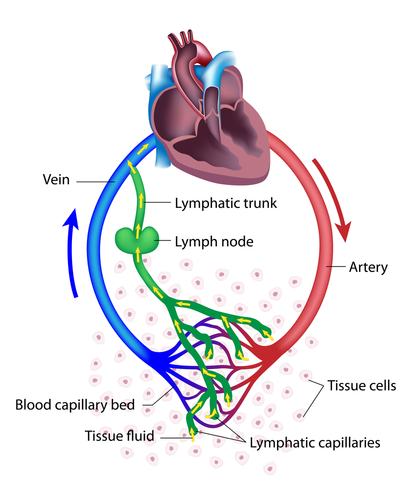
Your lymph system is a major part of your body's immune system. It’s made up of organs (spleen, thymus), lymph nodes, and lymph ducts and vessels. Together, they make lymph, collect it from tissues and carry it into the bloodstream.
Lymph is a clear to milky fluid that contains white blood cells (that attack bacteria in the blood) and fluid from your intestines (chyle) that contains fats and proteins.
Lymph nodes act like drains. They clean the debris out of the lymph as it passes through. If too much debris clogs the node, the lymph fluid doesn’t drain and the node swells and gets hard. (This is often called “swollen glands” but it’s really swollen nodes.) The blockage causes the lymph to backup and buildup, which eventually causes the area to swell. Sometimes the swelling develops quickly, or it may develop slowly over several months.
Lymphedema is an abnormal accumulation of protein-rich lymph fluid that typically occurs in the arm or leg, often the result of cancer treatments.
Lymphedema causes swelling (edema), chronic inflammation and fibrosis (thickening, hardening or scarring of the affected tissues). It can interfere with wound healing and cause severe damage to the skin.
Are you at risk for lymphedema?
Some factors increase your risk of developing lymphedema such as:
- Surgery for breast, gynecological, melanoma, head/neck, prostate or kidney cancer that includes removal of many lymph nodes
- Radiation therapy to areas that contain a lot of lymph nodes such as the neck, groin or armpit (You have hundreds of lymph nodes scattered throughout your body.)
- Certain drug therapies. Anthracyclines such as doxorubicin, taxanes such as paclitaxel and tamoxifen
- History of cellulitis, a bacterial skin infection that can spread and cause serious problems
- High body mass index (obesity)
- Tumor location
- Delayed wound healing
- Postoperative condition such as infection, hematoma (build-up of blood under the skin/bad bruise) or seroma (build-up of clear fluid under the skin near the surgery site)
What you can do
You can take steps to prevent lymphedema or keep it from getting worse. Tell your doctor right away if you have symptoms such as swelling of an arm, leg or other area; a limb that feels heavy or tight; you can’t move the affected limb as well as an unaffected limb; the skin on the limb is getting hard or thick; you have recurring infections; or your clothing or jewelry feels tight even though you haven’t gained any weight. Managing lymphedema focuses on two things:
- Keeping blood and lymph flowing. Avoid wearing tight clothing or jewelry. While sitting, do not cross your legs and be sure to change your position every half hour. Do not apply heat to the swollen area. If your arm or leg becomes swollen, elevate it (above your heart if possible). Remember to have your blood pressure taken in the arm without lymphedema.
- Preventing infection. Keep your skin and nails clean and dry and use lotion to keep it moist. Do not get any injections, blood tests or needle sticks in an area with lymphedema. Don’t test water temperature using the limb with lymphedema – you may not feel how hot it is and damage your skin. Wear gloves when working in dirt or with raw foods. Use sunscreen when outdoors. For small cuts, clean the area, apply antibacterial ointment and cover with a band-aid promptly.
While at-risk people can incorporate risk-reduction measures into their daily lives, even the most watchful person has no guarantee that lymphedema will not occur.
How is lymphedema treated?
There is no cure for lymphedema once it is established. The main goal of treatment is to manage the condition, relieve symptoms and control swelling to prevent additional tissue damage.
Roswell Park Comprehensive Cancer Center's Lymphedema Care provides specialized treatment to reduce swelling and discomfort and prevent infection. In the early stages, when the swelling is mild, it often can be managed by techniques that encourage lymph flow such as compression garments and elevating the affected limb. For more severe swelling, treatment sessions may include manual lymphatic drainage, therapeutic bandaging, proper exercises, skincare instruction regarding specific lotions and soaps, and self-care tips to reduce lymphedema in the future.


