Roswell Park team develops strategy for early detection and intervention to prevent lasting side effects of treatment
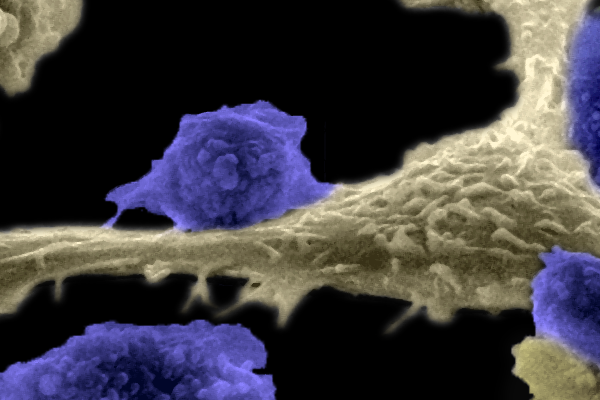
At Roswell Park Comprehensive Cancer Center, Philip McCarthy, MD, and a multidisciplinary team of colleagues recently undertook a study to understand how patients receiving CAR T-cell therapy were developing neurologic toxicity, a side effect that damages the nervous system and can result in limb weakness, memory or vision loss, headache and cognitive and behavioral changes.
Prior to this study, a 2019 consensus panel developed a grading system for cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) resulting from chimeric antigen receptor (CAR) T-cell therapy. This system has been important for identifying, treating and monitoring CRS and especially ICANS in CAR T-cell patients. ICANS is identified and monitored by the immune effector cell-associated encephalopathy score (ICE).
Therapists saw early warning signs
While patients routinely are evaluated using the ICE scoring system, the team found that some patients would have normal ICE scores and yet would have subtle differences in their ability to do more complex tasks, an early sign of ICANS.
“Two of our physical therapists, Hillary Jacobson and Renee McKenzie, astutely noticed some patients exhibiting subtle neurotoxicity symptoms prior to a change (decrease) in their ICE score,” Dr. McCarthy says. “ICANS, a serious complication of CAR T-cell therapy, can cause significant neurologic dysfunction if it is not recognized and treated.”
The study, he adds, was “truly a multidisciplinary effort, involving all members of our transplant and cellular therapy (TCT) team, starting with physical therapy, then inpatient nursing, led by Clinical Nurse Manager Laura Markel, who further evaluated neurologic function in our patients by monitoring for complex task completion, and then TCT nurse practitioners, physician assistants and physicians who further evaluated and prescribed treatment for our patients.”
The team described three patients with early neurologic toxicity and developed an evaluation tool to identify this toxicity earlier. That led them to develop a strategy for earlier intervention, and as a result, “we now are able to identify patients early in the development of neurologic toxicity, or ICANS, and initiate treatment to prevent further neurologic dysfunction during CAR T-cell therapy for hematologic malignancies,” Dr. McCarthy notes.
Because Roswell Park treats grade 1 ICANS, identifying early neurotoxicity symptoms is important. In addition to patients’ decreased ability in performing complex tasks, the team found changes in their personality, occupational confusion and inability to answer two-part questions to be early signs of neurotoxicity.
Another consideration was the difference in how adult brains and pediatric brains behave. Children who are being treated with CAR T-cell therapy have more resilience, are likely to rebound more quickly than adults and may not need early or as aggressive therapy for ICANS.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!Three-step strategy helps clinicians treat neurotoxicity earlier
The team’s strategy includes a three-step command tool to supplement the ICE score. They propose that CAR T-cell patients be consistently followed by clinical care providers (including family members) familiar with the patients to recognize early changes in personality, behavior and cognition. Additionally, they propose the tool be used in conjunction with the ICE score to detect early symptoms of ICANS. Early intervention has the potential to prevent significant and/or irreversible neurotoxicity.
“This strategy will allow us to identify toxicity earlier, treat it and avoid long-term complications of prolonged immunosuppression with glucocorticoid treatment with drugs such as dexamethasone and methylprednisone,” according to Dr. McCarthy.
“The key takeaway is that while we still don’t understand the complete pathogenesis of neurologic dysfunction after CAR T-cell therapy, if we can identify ICANS earlier, we hopefully will develop early treatment approaches. Most importantly, we need to understand the basis of this toxicity and develop strategies that will prevent it.”
The team plans to evaluate pre-clinical models of CAR T-cell therapy, investigate plasma biomarkers and clinical brain-imaging techniques for early detection and treatment of ICANS.