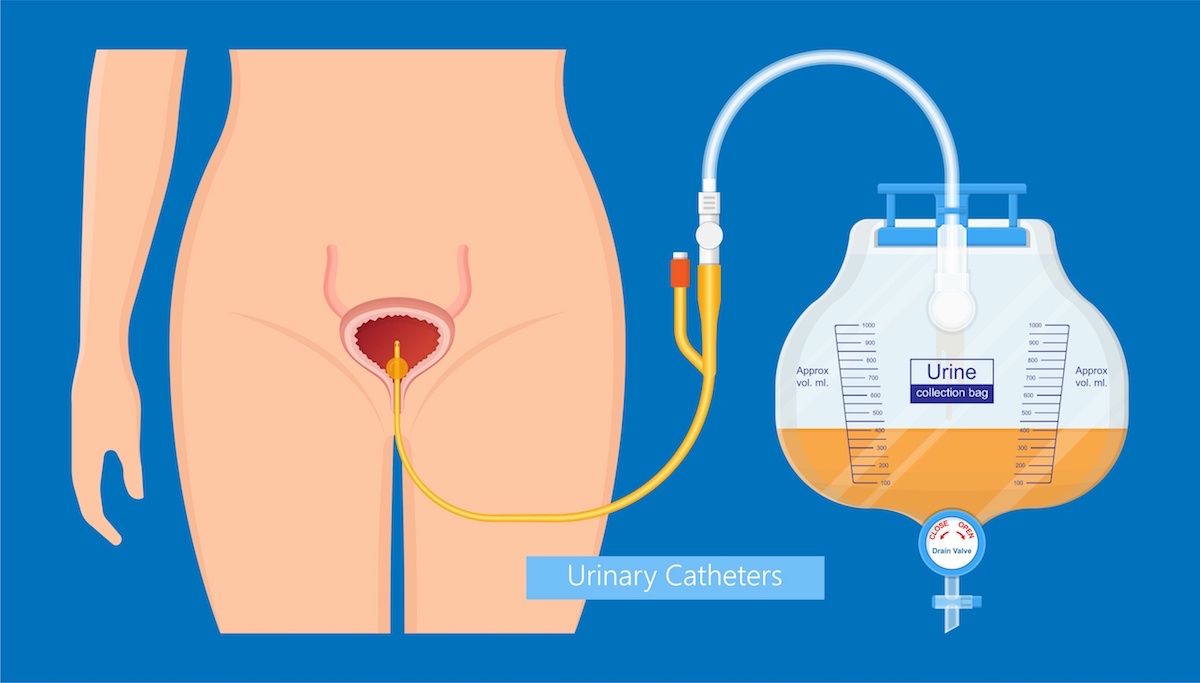
A Foley catheter is a semi-flexible plastic tube. One end is inserted into the bladder and the other end is attached to a bag that collects urine. It is used when you cannot urinate normally. This may be due to:
- Incontinence: You can’t control when you urinate.
- Urinary retention: Your bladder becomes full of urine and you (may) feel a desperate, urgent need to urinate, but you can’t. This is a concern because if urine remains in your bladder, you can develop a urinary tract infection. And although the bladder walls are muscular and can stretch, if they remain expanded for too long, the muscles will no longer be able to relax and you will not be able to urinate at all. Without relief, urinary retention can even lead to a bladder rupture.
- Urological or gynecological surgery that affects the bladder — for example, surgery involving the prostate, bladder, kidney or uterus.
- Anesthesia and opioid (narcotic) medications: These drugs can affect the nerves and muscles that control the bladder and urination, causing urinary retention and the need for catheterization. This happens more often in elderly patients. If you have had this problem in the past and you are being scheduled for surgery, be sure to let your doctors know.
- Medical conditions — for example, an enlarged prostate in men, a narrowing of the urethra (the tube that carries urine from the bladder to the outside of the body) and coma.
- Injuries — for example, spinal cord injuries.
- Input and output (I & O): Sometimes your clinical team needs to measure how much fluid you are taking in and how much fluid is going out. If you cannot use a commode with a collection/measuring device, collecting urine in a drainage bag provides an easy way to measure what is going out.
What to expect
People have mixed reactions to getting a urinary catheter. On one hand, while putting the catheter in place — or replacing it — may not be painful, it can be uncomfortable or embarrassing for some. On the other hand, urinary retention can be very painful, and inserting a catheter can provide great relief. If incontinence is the issue, a Foley can avoid problems that arise from having no control over your urination.
A Foley is considered a long-term or “indwelling” catheter because it can be left in place for a while. How long it will stay in place depends on your individual circumstances. Your physician will decide when to remove it or how often to change it. For example, if you are prone to catheter infections or blockages, it’s likely you’ll have the catheter replaced more frequently.
Catheters are among the most-used medical devices in hospitals. The most common complication with catheters is an infection called CAUTI (Catheter-Associated Urinary Tract Infection). The risk of developing CAUTI increases the longer a catheter is in place. To lower this risk, most catheters in hospitalized patients remain in place for only two to four days. After surgery, the catheter is removed as soon as you can urinate on your own.
What you can do
If you’re in the hospital, your nurses will care for your Foley catheter. If it’s left in place when you go home, follow the discharge and catheter care instructions you were given.
To help prevent infections and irritation or damage to the urethra and bladder:
- Wash your hands before and after handling any part of the Foley equipment.
- Drink six to eight glasses of water a day, unless you are on a fluid-restriction diet. Your urine should be clear or pale yellow.
- Clean the area where the catheter exits the body, and the catheter itself, with soap and water every day.
- Do not pull on, clamp, puncture or cut the catheter.
- While the catheter is in place, you may have bladder spasms, which can cause pain. Spasms are often set off by having a bowel movement. To help prevent spasms, use stool softeners to avoid constipation. Tell your doctor if you are having painful spasms. To lower risk of infection, clean the area well after having a bowel movement.
- Tell your doctor if you have any signs of infection, such as a fever of 100.4° F (38° C) or if urine is not draining into your bag. Your discharge instructions will specify when you should call the clinic.
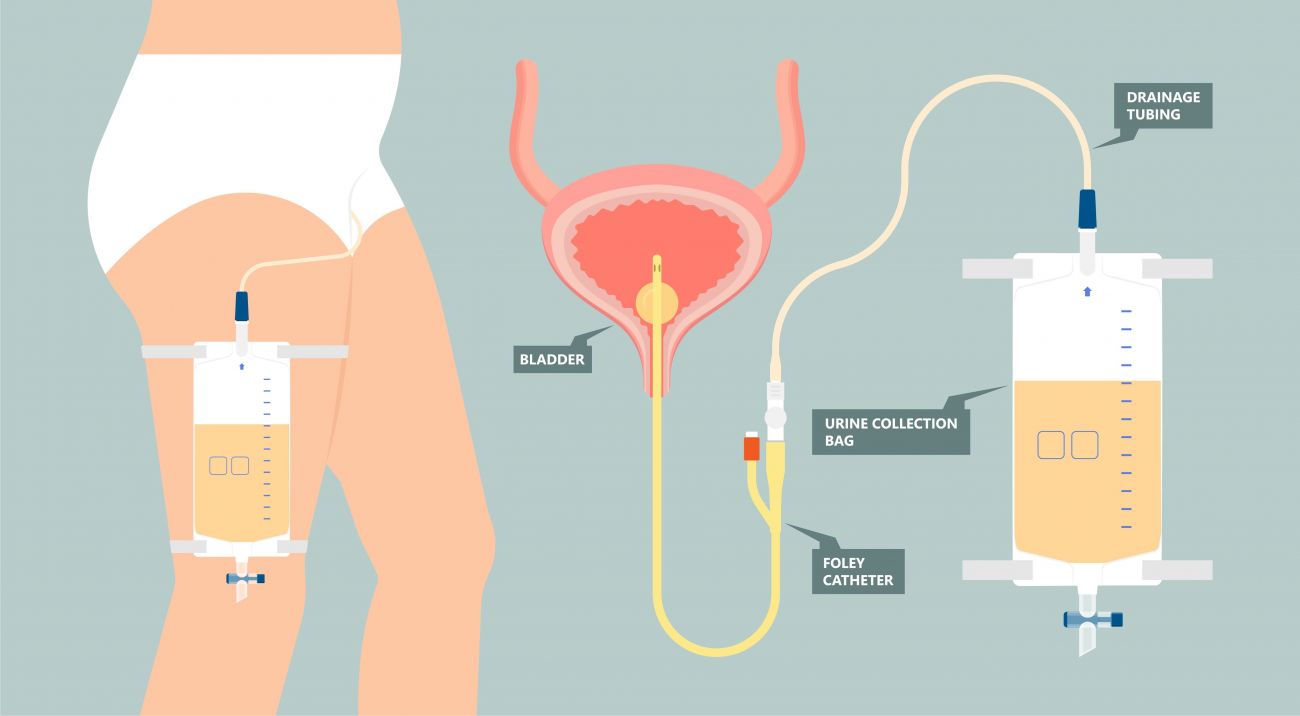
- There are two types of collection bags — a large one that can be hung on a lower bedrail and a smaller one that can be strapped to your leg and hidden under clothing if you need to move around or go out. Both types of bags must be kept below the level of your bladder. This prevents urine from flowing back into the bladder and reduces the risk of infection. Empty the drainage bag when the bag is half full. DO NOT allow the urine to sit in the bag for more than three to four hours.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!How is a Foley catheter put in place?
1) After explaining the procedure to you, a nurse will use a catheter kit to place your Foley.
2) The area around the urinary opening is cleansed. (The nurse may use an anesthetic gel to reduce any discomfort.)
3) The tip of the catheter is lubricated and inserted. Take deep breaths and try to relax.
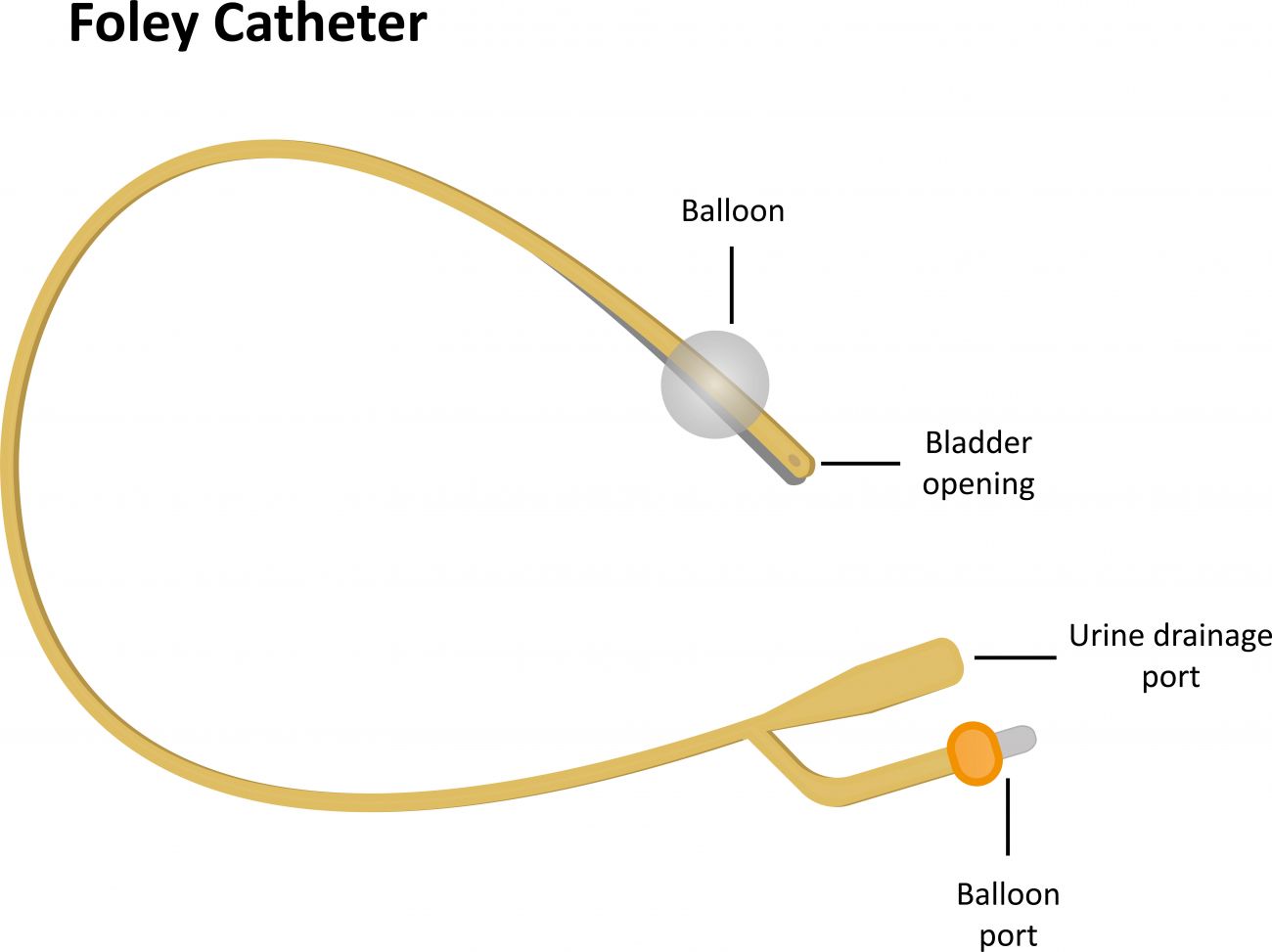
4) The tip of the catheter, which is inside the bladder, has a small balloon at the end so the catheter won’t fall out. Once the catheter is in place, the nurse will inflate the balloon through a special port. (The balloon will be deflated just before the catheter is removed.)
5) The catheter is then connected to the drainage bag.
Keeping the catheter working properly and preventing infection are the most important things you can do. Follow the instructions provided by your nurses to stay safe and recover as quickly as possible.