Peripheral neuropathy, or PN, is a condition that can cause weakness and unpleasant sensations in your hands or feet, or sometimes in other parts of your body. It’s caused by damage to the peripheral nerves — the nerves located outside of the brain and spinal cord.
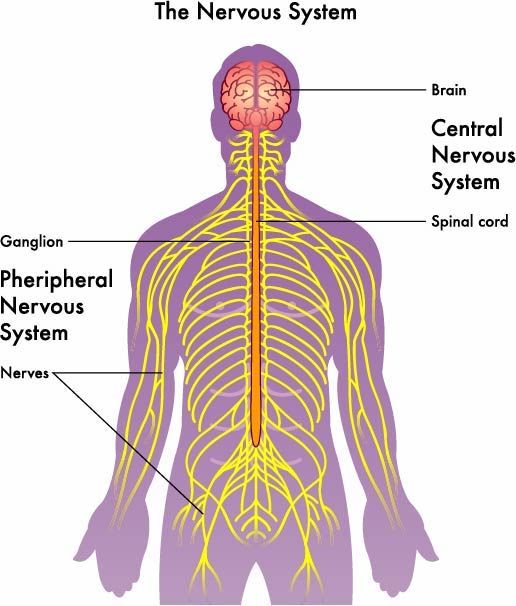
The brain and spinal cord make up the central nervous system. The peripheral nervous system connects your central nervous system to your organs and limbs. Peripheral neuropathy may be caused by some medications prescribed for seizures, high blood pressure or cancer. It can also be caused by disease itself, such as cancer and diabetes.
Chemotherapy-induced peripheral neuropathy (CIPN) is a specific type of PN. It's caused when chemotherapy drugs cause harm to nerve cells by damaging their structure and/or their ability to function as they should.
About peripheral nerves
There are three main types of peripheral nerves:
- Sensory nerves, which help you feel touch, pain, temperature and position
- Motor nerves, which help you move and maintain muscle tone
- Autonomic nerves, which automatically regulate such body processes as breathing, heartbeat and digestion
Most neuropathies affect the sensory nerves, but motor and autonomic nerves can also be affected.
Possible symptoms of peripheral neuropathy
- Tingling, “pins & needles,” numbness
- Burning, discomfort, sharp pains
- An unpleasant sensation when touching or being touched
- Inability to sense heat or cold
- Weakness
- Trouble picking up or holding objects
- Problems with balance or walking (clumsiness)
Who is at higher risk for CIPN?
The risk factors below may make it more likely for you to get CIPN. Having one or more of these factors doesn’t mean you will get PN; everyone is different. There are people who have a few risk factors and don’t get PN, and others with no risk factors who do.
Drug and dose: The total amount of CIPN-inducing drugs you received is high. You had high doses of CIPN-inducing drugs at each infusion.
Age: Older people are at higher risk.
Preexisting conditions: Neuropathy began before chemotherapy, or it was caused by the cancer. Poor kidney function means it takes longer for the body to get rid of creatinine, a waste product created by the muscles.
Personal history: History of smoking or exposure to other agents that are toxic/harmful to nerves.
What anti-cancer drugs are most likely to cause CIPN?
- Platinum-based drugs: cisplatin/Platinol®, oxaliplatin/Eloxatin®, carboplatin/Paraplatin®
- Taxanes: paclitaxel/Taxol®, docetaxel/Taxotere®, cabazitaxel/Jevtana®
- Thalidomide and its relatives: carfilzomib/Kyprolis®, lenalidomide/Revlimid®, pomalidomide/Pomalyst®, apremilast/Otezla®
- Epothilones: ixabepilone/Ixempra®
- Proteasome inhibitor: bortezomib/Velcade®
- Vinca alkaloids: vincristine/Marqibo®, vinblastine/Velbane®
The neuropathy caused by most of these drugs commonly shows up weeks or months after treatment has ended. Paclitaxel and oxaliplatin are exceptions; they can cause neuropathy during or immediately after infusion.
Your doctors and nurses will do all they can to minimize the risk while maintaining the effectiveness of your treatments. Unfortunately, right now there is no way to completely prevent PN. Research studies continue to search for ways to prevent and treat peripheral neuropathy.
Frozen socks and gloves? The search for answers
These medications/agents have been studied as possible ways to relieve CIPN: anti-seizure drugs, antidepressants and some high blood pressure drugs; glucocorticoids (steroids); neuro and chemo protectants; hormones; amino acids; vitamins; copper-chelating agents; supplements; enzymes; electrolytes (calcium/magnesium); omega-3s; cold; longer infusion time; and exercise.
After reviewing mixed results of clinical trials and pilot studies, the American Society of Clinical Oncology (ASCO) determined that there was not enough evidence to recommend that patients receive any of the tested agents to prevent CIPN or lower the risk of developing it.
ASCO says some agents should not be given to patients, because they made the CIPN worse or caused unacceptable side effects: acetyl-L-carnitine, amifostine, amitriptyline, calcium/magnesium infusions (for oxaliplatin patients), gluthathione, nimodipine, retinoic acid, recombinant human leukemia inhibitory factor (rhuLIF) and vitamin E.
A few agents look promising, but more research is needed before ASCO can make any recommendations about them. They include carbamazepine, glutamate, goshajinkigan, omega-3 fatty acids and venlafaxine.
Studies showed that using frozen socks and gloves before, during and after infusion may lessen symptoms, and exercise may offer some protection from CIPN. Again, these are early reports, and there is not enough evidence to recommend their use at this time.
To treat existing CIPN, ASCO recommends the prescription antidepressant duloxetine. In the U.S., it is sold under the brand names Irenka® and Cymbalta.®
What can I do to relieve my CIPN?
- Do not take any medications or supplements that have not been prescribed by your doctor.
- Walking, low back stretches and calf stretches can help keep your muscles flexible.
- Try foot and hand massages to relieve stiffness. Clean lotions and creams off afterward.
- You can buy special equipment in health supply stores to help you dress: zipper pulls, buttoners, etc., and special pens, pencils and utensils that are easier to hold.
- Wear shoes that go over the insteps of your feet.
- Wear gloves and warm socks in cold weather.
- Avoid alcohol and drugs that may affect your balance, coordination or alertness.
How can I reduce my risk of injury?
If you have lost feeling in your hands or feet, you’ll need to rely more on your vision. Here are some safety tips:
- Be sure you can see well anywhere you walk or do activities.
- Keep switches and lamps at entrances so you can light a room before you enter it. Keep a flashlight with you. Put a light on your keychain. Use nightlights along paths you may walk at night — for example, to the bathroom or a child’s room.
- Put handrails on both sides of all stairways and hallways.
- Cover stairs and floors with a non-glare, non-slip surface.
- Remove all the clutter from stairways and hallways.
- Wipe up spills immediately.
- Tape or tack down carpet and rugs. Mats should have a non-slip backing.
- Do not use chairs, stands or tables with wheels.
- Because you have reduced feeling in your hands and/or feet, you are at risk for heat injuries. Ask someone to test the water temperature before you put in your hand or foot.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Does CIPN get better after chemotherapy?
For many people, yes. As mentioned, in most cases CIPN symptoms build gradually, getting worse with each infusion. Symptoms flare up right after the infusion and calm down by the next dose. It is common for symptoms to peak about three to five months after the last dose of chemotherapy. Afterward, symptoms may gradually lessen in intensity, disappear or affect fewer areas of the body. Unfortunately, for some survivors, CIPN becomes permanent.
Researchers at the Oregon Health Sciences University conducted a study of CIPN in 513 female cancer survivors — mostly breast cancer patients, with an average age of 62. They found that 47% reported CIPN symptoms six years after the end of treatment. They walked slower, had a higher level of disability and were more likely to fall, and their quality of life had suffered. The researchers also observed that early interventions, such as exercise programs and asking patients about their CIPN symptoms, seemed to help preserve the patient’s quality of life during and after treatment. The researchers wondered if early intervention is helpful because providers have shied away from discussing CIPN with their patients because of a lack of treatment options to offer.
Where can I turn for help?
- Ask your nurse for a copy of the Patient Education brochure “Peripheral Neuropathy,” or pick up a copy in the Patient & Family Resource Center on the first floor of the hospital, inside the Sunflower Café. You can find it online in the Patient Education Library in the patient portal (MyRoswell).
- Your doctor or nurse may have specific suggestions.
- Physical and occupational therapists can help with exercise programs and adaptive devices for work or home.
- You may wish to have a podiatrist care for your feet.
- The Foundation for Peripheral Neuropathy can provide general information and help locate a support group. Call 1-877-883-9942.
- The Neuropathy Action Foundation promotes awareness, education and empowerment for those with neuropathy, regardless of what caused it.