Before her breast cancer diagnosis at 42, Sara Sade wasn’t aware that being an Ashkenazi Jew increased her risk of getting cancer.
She didn’t find out until a few months later, when her sister was diagnosed with ovarian cancer. That's when Sara’s doctor told her, “You need to have genetic testing.” Three years later, in 2010, Sara got a second cancer diagnosis — melanoma.
Ashkenazi Jews are people whose Jewish ancestors came from Central or Eastern Europe. Genetic mutations passed down from generation to generation in this group are responsible for higher-than-average rates of cancer. The risk is linked mostly to these four genes:
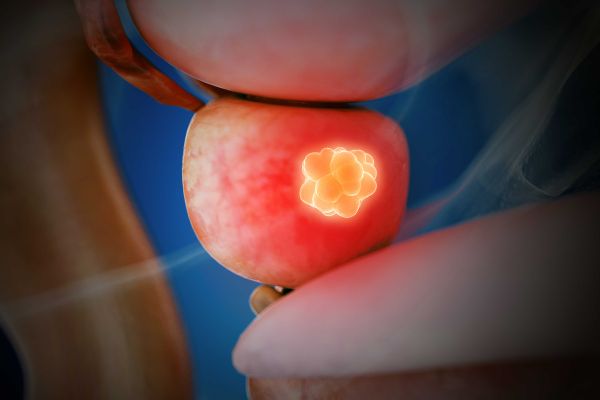
- BRCA1 and BRCA2, linked to
- Breast cancer and ovarian cancer in women
- Breast cancer and prostate cancer in men
- Melanoma
- Pancreatic cancer
- About one in every 40 Ashkenazim has a BRCA mutation; in the general population, the rate is about one in every 400 people.
- GREM1, linked to colon cancer
- APC, linked to colon cancer
“If we do genetic testing primarily because of someone’s Ashkenazi Jewish ancestry, those are the Big Four genes we'd think about,” says Katherine Latina, MS, CGC, Genetic Counselor with Roswell Park’s Clinical Genetics Service. “But if there are a lot of breast cancers or ovarian cancers in the family, we want to cast the net a bit wider with testing. I’d hate for someone to be tested for only four genes, when maybe there is another gene mutation we should be worried about, but we never looked there. So we take their personal and family medical history into account, in addition to their ancestral background.”
Sara underwent genetic testing in 2007 — the year of her sister’s diagnosis — and again in 2015, when she first came to Roswell Park after her melanoma had metastasized throughout her body. (Repeated tests are necessary to keep up with discoveries of new cancer-related genes.) Both times testing showed that she did not have the gene mutations normally associated with cancer risk in Ashkenazi Jews.
Even so, her family medical history showed a clear risk pattern. She was advised that although her risk is due to an inherited gene mutation, the specific cancer-related gene has not yet been discovered.
Genetic Screening at Roswell Park
Get more information about the genetic screening process.
High-Risk Screening
Armed with the knowledge of her own potential cancer risk, Sara’s older daughter, Emma Vangelista (shown above on her wedding day, with her mother), had her first screening mammogram last fall through Roswell Park’s high-risk breast cancer clinic. At 32, she’s 13 years younger than the recommended age when women at average risk should begin breast cancer screening. But women in the high-risk group are advised to begin screening 10 years before the age at which their youngest close relative with breast cancer received the diagnosis.
“Every November I’ll have a normal bilateral mammogram [both breasts], and every May I’ll have a breast MRI and a right-sided mammogram, because they found a cyst on my right side,” Emma explains. “Everything’s fine, but they want to keep track of it because of my family history.”
Emma also plans to undergo genetic screening and testing, so right now she’s working with her mother to fill in the blanks about their family history of cancer. Thinking about the possible test results is “a little nerve-wracking and scary,” she admits, but understanding her risk also gives her a sense of control over the situation, because she’s taking steps that could help find cancer earlier if it does develop.
Understanding and Managing Cancer Risk
How big a role do inherited gene mutations play when it comes to cancer risk? Latina says that in general, “most cancers seem to be just random, sporadic occurrences. Inherited cancer-related mutations are pretty uncommon.”
She cautions that even if genetic testing shows that you have an inherited cancer-related mutation, “it doesn’t mean you’ll definitely get cancer. Your risk is just higher than that of the average person. For example, women in the general population have about a 12% risk of developing breast cancer in their lifetime. Having a BRCA mutation might bump that to a 50%-60% lifetime risk. It’s a big jump, but it’s not 100%.”
Those at high risk may consider a range of strategies to manage their risk. “We spend a lot of time with people talking about what feels like the best option for them,” says Latina. That can range from more frequent or intensive screening procedures (colonoscopies for colon cancer, skin exams for melanoma, imaging for pancreatic cancer or mammograms for breast cancer, for example) to risk-reducing surgery — surgical removal of the breasts or ovaries, depending on the type of cancer risk.
The Importance of Knowing and Sharing Your Family Medical History
To give genetic counselors the information they need to determine whether genetic testing might benefit you or your family, it’s important to know which of your relatives were diagnosed with cancer, what types of cancer they had, and at what age they got the diagnosis. “Gather the information you can from your family members,” Latina advises. Death certificates and other records can provide additional information. Latina says it’s important to let your healthcare providers know about that family medical history.
Sharing the same information with your family members can help them make decisions about determining their own cancer risk. That’s just what Sara Sade and Emma Vangelista have done. And when Emma’s younger sister, Alanna, turns 32, she’ll follow in Emma’s footsteps with breast cancer screening.
You Should Know
- Roswell Park patients who want to learn more about genetic testing should speak with their Roswell Park providers. Anyone outside Roswell Park can ask their primary healthcare provider to place a referral for a genetic consult, or self-refer by calling 1-800-ROSWELL (1-800-767-9355).
- New guidelines from the National Comprehensive Cancer Network (NCCN) released in December 2019 recommend that all pancreatic cancer patients receive genetic testing, especially because “their at-risk family members could greatly benefit from known, effective cancer-risk-reducing interventions.”
Editor’s Note: Cancer patient outcomes and experiences may vary, even for those with the same type of cancer. An individual patient’s story should not be used as a prediction of how another patient will respond to treatment. Roswell Park is transparent about the survival rates of our patients as compared to national standards, and provides this information, when available, within the cancer type sections of this website.