When a scientist becomes a cancer patient
Frank Price, PhD, thought he had appendicitis when he took himself to a hospital in Utica, NY, with pain in his abdomen nearly four years ago. “But after tests proved otherwise, I was relieved to be sent home,” recalls the 73-year-old biologist, whose 50-year career has included teaching and research in ecology, biology, anatomy and physiology.
But when the pain persisted, he returned to the emergency room the next day. After two weeks in the hospital with inconclusive tests, surgeons discovered a neuroendocrine tumor (NET) in the wall of his small intestine. “I’d never heard of neuroendocrine cancer,” he says.
NETs behave differently than most cancers. They typically arise from nerve and endocrine cells in the lungs, pancreas, intestine and sometimes other organs. They grow slowly and initial symptoms are usually caused by oversecretion of hormones. Small tumors and metastases can be difficult to detect and don’t typically respond to chemotherapy. Frank’s tumor was determined to be carcinoid, a subtype of neuroendocrine tumor.
Although the diseased section of Frank’s small intestine was removed, his cancer had metastasized around major blood vessels and into his liver. He underwent surgery, embolization treatments and, for two years, monthly injections of Sandostatin, a hormone-like drug that eases symptoms caused by the overproduction of hormones. But last year, when CT scans showed more liver tumors, Frank began to look for other options, which brought him to Roswell Park Comprehensive Cancer Center.
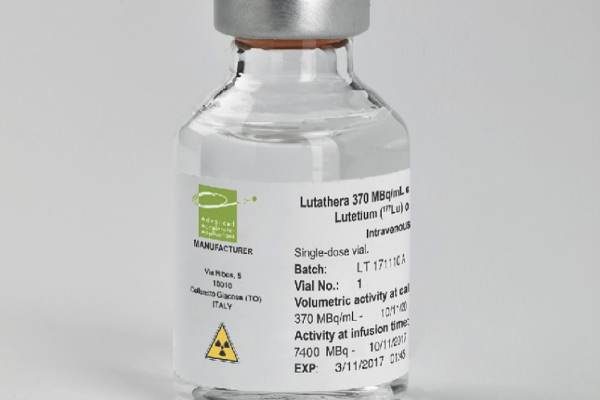
Frank’s scientific background makes it easier for him to be an active partner in his treatment. “I’m a researcher by nature, so I’m always curious, looking at options, reviewing reports and following up with doctors when I have questions,” he says. “I learned that Roswell has a newer gallium scan, a type of nuclear medicine exam that can detect very small carcinoid tumors better than alternative imaging.” In addition, tumors that are identified by this scan are able to be treated with peptide receptor radionuclide therapy (PRRT), a treatment that uses a synthetic hormone (which is tagged with radiation) to find cancer cells, attach to them and deliver radiation directly to the cells. “The scan found I had metastases in a shoulder blade, and in my lungs, abdominal lining and pelvis. Traditional chemo doesn’t affect NETs, so I spent the next eight months receiving PRRT.” Learn more about the Netspot Scan (Gallium-68 dotate).
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
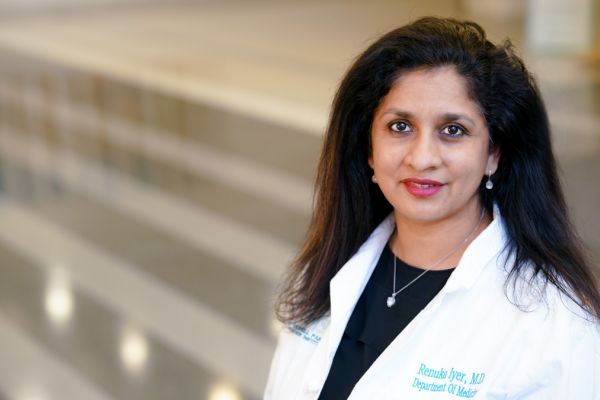
Sign up!Frank’s interest in the science of his own cancer broadened his own knowledge base. He recalls a meeting he and his wife, Sue Ann, a developmental cell biologist and anatomy professor, had with Renuka Iyer, MD, founder of the Roswell Park Neuroendocrine Tumor Biobank and Chief of GI Oncology at Roswell Park. “Our questions prompted Dr. Iyer to take out a pen, start drawing diagrams and launch into a 20-minute lecture on developments of clinical trials and research,” he says. “We were thrilled to learn. Dr. Iyer and my doctors at Roswell pretty much gave us a graduate course in neuroendocrine tumors.”
Frank’s advice to patients, even those who aren’t scientists?
- Always ask for copies of pathology and lab reports, doctor’s reports and surgical notes. “I live three hours away from Roswell, so I always request paper copies to review and make notes when I’m back home. I bring them to doctor visits to be sure I remember all my questions.”
- Knowledge is very important for your mindset during treatment. “It’s especially important for patients who don’t have a scientific background to be sure to ask questions of their doctors and to be sure they understand the answers.”
- Take advantage of support groups and online resources to educate yourself and become a better partner in your care. “Having support makes a difference. I’m fortunate that my wife, Sue Ann, comes with me to all my appointments at Roswell.”
Frank’s treatments and monitoring will continue. “We’re keeping track of how far the tumors have spread. I’ll continue to get monthly Sandostatin injections, periodic scans and I may be a candidate for more PRRT. I really have no major symptoms. I don’t get ‘carcinoid syndrome,’ where you can get severe diarrhea, facial flushing and heart valve damage,” says Frank.
“I sometimes get loose stools as I get close to needing injections. Some of the changes that I thought were part of aging were actually the early stages of carcinoid syndrome. I wonder at times if I might be flushing. It’s described as similar to menopausal hot flashes, but my wife tells me, ‘You do NOT have hot flashes,’” Frank says with a chuckle.
Frank continues to enjoy an active retirement, hiking with Sue Ann, birding and highpointing, a hobby that involves visiting the highest natural ground in each county.
“I’m lucky I can drive around and hit the high points,” says Frank. “We’ve visited more than 640 of the 3,142 counties in the United States and I’m looking forward to reaching many more.”
Editor’s Note: Cancer patient outcomes and experiences may vary, even for those with the same type of cancer. An individual patient’s story should not be used as a prediction of how another patient will respond to treatment. Roswell Park is transparent about the survival rates of our patients as compared to national standards, and provides this information, when available, within the cancer type sections of this website.