When Avoiding Full Disclosure Could Have Serious Consequences
It probably comes as no surprise to hear that alcohol and cancer do not make for a happy or healthy couple. But what if you or someone you know already had a preexisting relationship with large amounts of alcohol, before they were diagnosed with cancer?
If you are undergoing treatment, it’s important to stay informed of the risks that alcohol may bring to your outcome. Equally important to recognize are the risks and possible side effects of going through withdrawal symptoms if you follow your doctors’ directions to reduce or eliminate alcohol from your routine, while in treatment.

Unfortunately, due to social stigmas associated with alcohol dependence, it can be common for some patients to withhold information about the quantity and frequency of what they are drinking. “I have found that some patients find it difficult to fully disclose their alcohol use due to many factors, but the most common reason is that they do not want friends or family to know,” says Medical Social Worker, Joni Maxick-Jason, LCSW.
Maxick-Jason says that underestimating alcohol consumption can be common for many people who abuse alcohol, as they may not consider the amount of alcohol they drink as dependent behavior. “I have had some cases where patients have disclosed consuming minimal quantities of alcohol but after full assessment, we came to find out it was much greater. This is a very delicate subject and we always let patients know we are here to support them in any way we can,” says Maxick-Jason. “Joining with patients early in their assessment and assisting them in obtaining necessary resources typically results in better outcomes, and it may also help avoid embarrassment that could lead to patients missing important medical appointments.”
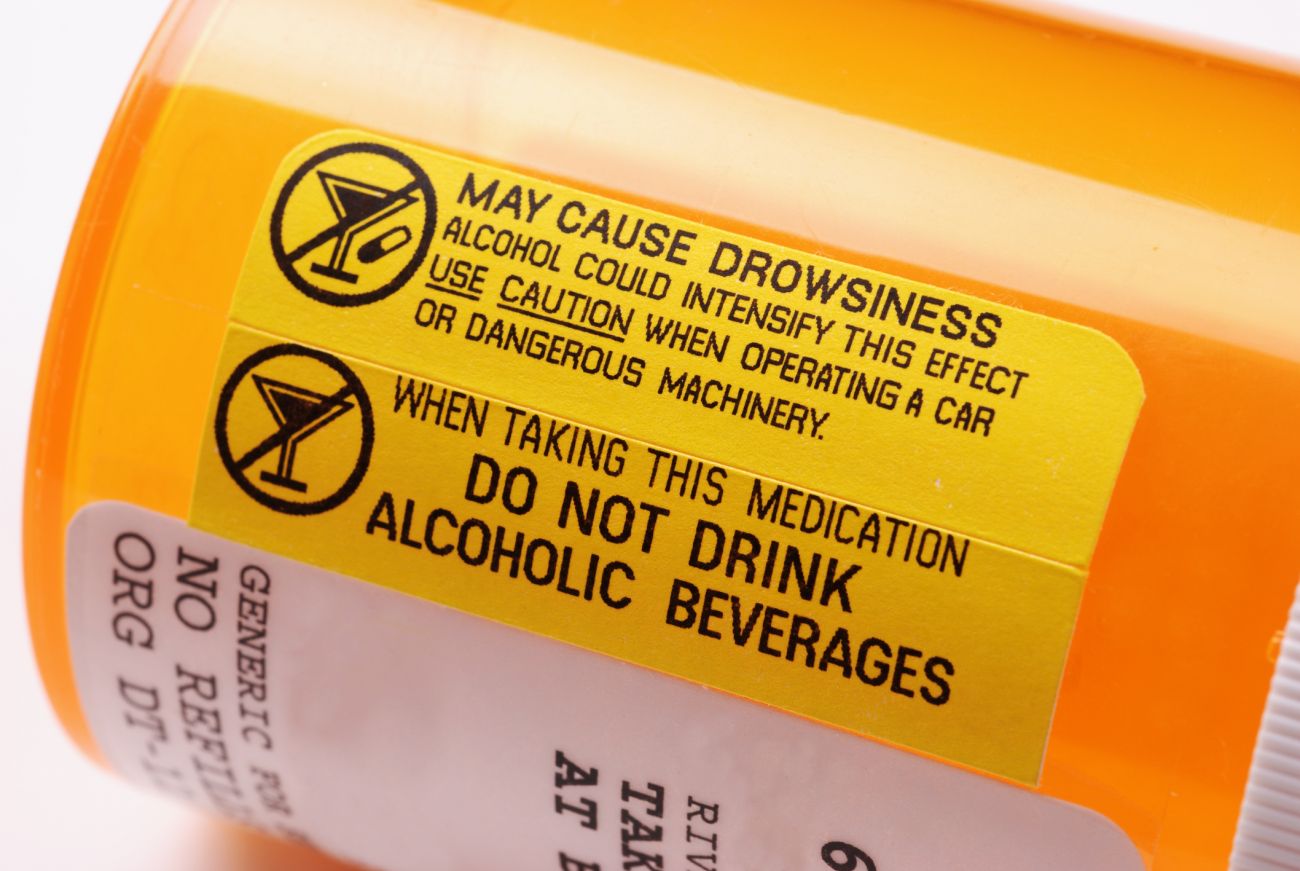
It’s imperative to understand that avoiding full disclosure could have serious consequences. Chemotherapy, medication and radiation treatments will change how the body works. Adding toxic substances such as alcohol during this process will affect the effectiveness of medications, can complicate surgery outcomes and may also influence the body’s ability to heal. While some people mistakenly believe that it’s safer to drink certain types of alcohol rather than others, all alcoholic drinks contain the same key substance, ethyl alcohol or ethanol, and it’s the quantity and frequency of consumption that will influence treatment and recovery.
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!Maxick-Jason notes that for most patients, the main focus is usually on his or her cancer and getting through treatment. But she stresses that if past coping mechanisms included alcohol use, that use could increase if not addressed. Social workers at Roswell Park will assist patients in locating community resources where they can receive substance abuse assessment and continuing treatment. To reinforce support, social workers may ask patients to sign releases allowing communication between outside rehab providers and the Roswell Park team, allowing for a better continuum of care.
It’s critical that patients realize that the more open they are with their care providers, the better Roswell Park staff can help them achieve the best possible outcomes for their treatment, surgery, and ultimately, recovery. Doctors also need to know if a patient is alcohol dependent because suddenly eliminating alcohol could cause withdrawal symptoms such as tremors, confusion, hallucinations, seizures, and other serious problems which could complicate surgery and medication protocols.
“The more forthcoming a patient can be in the beginning, the more successful we can be in getting them the resources they need, whether it be assisting in referrals to a detox program, outpatient care, or counseling to work on healthy coping skills,” says Maxick-Jason. “Ultimately we are here without judgment, to help our patients’ experiences be as safe and effective as possible. We'll help them get the support they need to cope with the mental stress of having cancer, so that they can have the best possible outcomes.”