Polycystic ovary syndrome increases risk for other health conditions, including uterine cancer
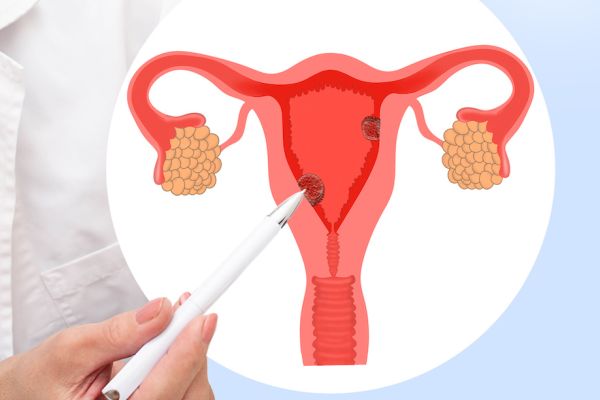
Polycystic ovary syndrome (PCOS) affects as many as five million women in the United States. This common hormonal condition occurs when small, fluid-filled sacs — called cysts — form on the ovaries. While many women with PCOS experience no symptoms, the condition is sometimes associated with hormonal imbalances that increase the risk of certain health problems, including uterine cancer.
“Simple ovarian cysts in isolation are not known to be precancerous or increase the risk of ovarian cancer. However, PCOS as a syndrome is associated with infertility, obesity, chronic lack of ovulation, hormonal imbalances and chronic low-grade inflammation. Some studies suggest a small increased risk for ovarian cancer as a result of these associated conditions, but other studies fail to identify a connection,” says Peter Frederick, MD, FACOG, Clinical Chief of Gynecology at Roswell Park Comprehensive Cancer Center. “However, we do see an increased for uterine cancer with PCOS.”
Uterine cancer is the fourth most common cancer for women in the United States, and endometrial cancer, cancer of the uterus lining, is the most common uterine cancer. “The lifetime risk of a woman developing uterine cancer is about 3%. But for women with PCOS, that risk increases to around 8-9%,” explains Dr. Frederick.
Polycystic ovary syndrome tends to run in families. The disruption of hormones caused by the syndrome also can lead to insulin resistance, rising blood sugar levels and increased risk for type 2 diabetes.
Treating PCOS can help reduce cancer risk
One of the most common treatments for PCOS is oral contraception, which helps regulate menstrual cycles. “Bringing hormones back into a healthy range with oral contraceptive pills helps regulate estrogen and progesterone, and has the added benefit of reducing risks for certain cancers including ovarian and endometrial cancer,” notes Dr. Frederick.
Working with patients to help address the underlying causes of cancer is a priority. “You can’t treat cancer in a vacuum, you have to look at all the factors, including genetic predispositions and lifestyles. When it comes to reducing risks, maintaining a healthy diet and regular exercise not only results in better outcomes for endometrial cancer, but also reduces the risk of other conditions such as stroke and cardiovascular disease.”
Recognizing the strong connection between healthy lifestyle and better outcomes, Roswell Park is actively engaged in studies with patients. Fitbits are available to help people monitor their daily steps and activity levels and smartphone apps enable patients to participate in blood glucose monitoring. These observational studies help contribute insights into the complex interplay between physical activity and cancer outcomes.
You have time for a second opinion
A precise and accurate diagnosis, staging, and treatment plan by a team of experts who focus on uterine cancer every day, is essential.
Don’t ignore warning signs, risks
Symptoms for uterine cancer typically include abnormal bleeding, such as irregular and heavy bleeding between periods, as well as postmenopausal bleeding.
“Any irregular bleeding should always be evaluated. It doesn’t necessarily mean that cancer is present, but those symptoms should not be ignored and can be evaluated in an office visit with an endometrial biopsy. The earlier the cancer is identified, evaluated and treated, the better the prognosis," Dr. Frederick says.
If there's a strong family history of any kind of cancer, Dr. Frederick recommends discussions with a healthcare provider, who can look at your family history and make a recommendation for genetic testing. “Identifying inherited risk factors can be key to early detection and prevention.”
Comprehensive treatment for uterine cancer
“The gold standard for uterine cancer is a hysterectomy, where we remove the uterus and cervix,” says Dr. Frederick. “Depending on a patient’s age, we may also remove the ovaries and fallopian tubes at the same time.” However, fertility-sparing approaches may be an option for younger patients who hope to become pregnant. “We make recommendations on their cancer treatment and then work closely with fertility specialists to make recommendations about the timing of attempting a pregnancy, as well as any additional medical or surgical approaches that could increase the likelihood of a successful pregnancy.”
For patients who are not good candidates for a hysterectomy, options include progesterone treatments in the form of an oral tablet, injection or a progesterone-releasing intrauterine device. “Progesterone is more effective for low-grade uterine cancers and less effective for high-grade cancers. It may also be a better option when a hysterectomy is too risky or for women who want to maintain fertility,” says Dr. Frederick.
For patients who cannot safely undergo surgery, or those with advanced or recurrent cancer, other options are available. “Each patient’s treatment is always highly individualized. We're doing a lot of work with immunotherapy and using more targeted treatment approaches with patients who may have a more advanced stage or recurrent endometrial cancer. These new approaches have really pushed the envelope for long-term survival, and quality of life,” says Dr. Frederick.
Cancer care closer to you
You can access Roswell Park quality cancer care through our network of community cancer and specialized care providers, all throughout New York State.