For patients with multiple myeloma, the goal is to have as long a period of remission as possible.
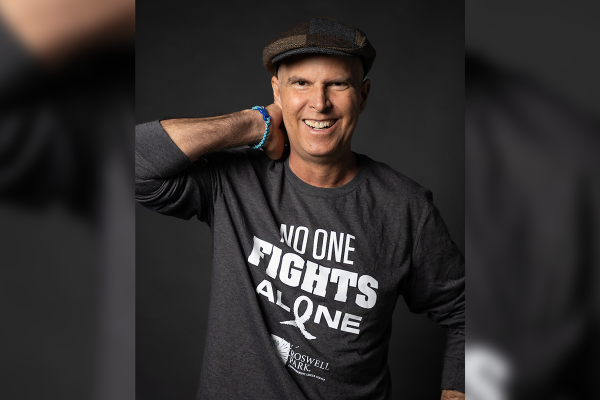
That’s why Roswell Park Comprehensive Cancer Center should be the first stop a patient makes after their diagnosis, says Hamza Hassan, MD, a hematologic oncologist and member of Roswell Park’s Multiple Myeloma Translational Research team and the International Myeloma Working Group (IMWG).
Multiple myeloma is a kind of blood cancer in which abnormal plasma cells — a type of white blood cell — multiply at an out-of-control pace. Unlike leukemia or lymphoma, there is no cure for multiple myeloma.
Historically, the first line of treatment has been a combination of three or four medicines that largely comprise newer treatments like immunotherapy. Immunotherapy harnesses a person’s own immune system to kill myeloma cells. This process achieves remission. To deepen the response or to prolong the achieved remission, oncologists would frequently recommend a stem cell transplant (formerly called bone marrow transplant). This stem cell transplant would involve collecting the patient’s healthy stem cells from their own bone marrow before chemotherapy, then putting them back in the patient’s body after a different kind of chemotherapy has successfully reduced the presence of multiple myeloma plasma cells. This whole process of three or four medicines induction with or without an accompanying stem cell transplant is termed as the first line of myeloma treatment. Frequently, this is the longest remission for most patients.
“The patient is their own donor in this kind of transplant, reducing the risk of complications like rejection,” Dr. Hassan says. “After they’re well enough, they will receive another round of the vaccines they received as children because their immune system will essentially be close to brand new.”
Things have changed in the past few years, he adds. Instead of waiting for a relapse to consider providing the patient with a stem cell transplant, he and other specialists now discuss transplants as part of a first line of treatment, among other options that didn’t exist previously.
“A majority of physicians who treat multiple myeloma recommend doing a stem cell transplant earlier because your first remission is the longest remission and typically the best one,” he says. “With each subsequent line of therapy, your duration of remission keeps getting shorter, though I have had exceptions in certain cases. The end goal is to have as long a remission as possible so they can enjoy living their life and exploring the world. You want to offer patients their transplant with their first line of therapy after we have knocked down the disease.”
Earlier transplant could mean longer remission
Having a transplant right away after initial combination therapy reduces the disease to low levels, if not immeasurable. The transplant prolongs the duration of initial remission by about one-third and results in long-term side effects only for a minority of patients.
“If someone was going to have a remission of three years, by having a stem cell transplant immediately following initial treatment, it becomes four years, and four years can become six years and so on,” Dr. Hassan explains. “Studies have shown up to two years of a longer remission, about 23 months, but that varies from patient to patient. What’s more interesting is the evidence showed patients who have a transplant also have a higher quality of life and they recover to a better level than those who didn’t have their transplant right away.”
You have time for a second opinion
Treatment focuses on getting you into remission, with minimal residual disease, and extending the duration of the remission — achieving this requires the knowledge of doctors who are experts in the field.
Comprehensive care helps improve quality of life
The timing of a patient’s transplant is ultimately up to the patient and their doctor. However, specialists at a comprehensive cancer center like Roswell Park are best equipped to advise on this course of treatment because they treat more multiple myeloma cases than other hospitals.
“Having the lens of judging and making the determination can only happen with the multidisciplinary approach at a comprehensive cancer center,” Dr. Hassan says. This provides the support patients need before, during and after treatment, including nutritional support, pain management, physical therapy, a dedicated pharmacist specializing in oncology, radiation and into survivorship as they learn to navigate life with multiple myeloma.
“We want them to know what to do when myeloma is in remission and preparing for when it comes back, because our research is still not perfect; we are still trying to cure it, but the only way to most effectively treat it is by keeping the patient in the best state possible,” advises Dr. Hassan, who likes to bring up transplants as a course of treatment as soon as possible.
“We have to empower the patients with why this is a good course of treatment,” he explains. “If I’m telling someone their quality of life is going to temporarily diminish, I need to give them reasons why I think this is the best way to go in the long run. This is an investment that will give you a good return, longer remission, with better quality of life. Those two things are important.”
This also applies to patients who are initially treated somewhere other than Roswell Park but come in for a second opinion or consultation.
“They are the ones who need the focused planning for this process so we can coordinate with their other local doctors,” Dr. Hassan says. “It’s a win-win situation where we can give the comprehensive care to patients who might receive their primary care closer to home. We all have the same goal. We want our patients to get better care, have fewer symptoms, have longer remission and better overall quality of life.”