This is the first in a series of three Cancer Talk blogs about a new immunotherapy developed at Roswell Park that is now being studied in patients who are enrolled in a phase 1 — “first in human” — clinical trial. It marks the first time a patient has received this specific type of adoptive T-cell therapy anywhere in the world. It also marks the first time Roswell Park has produced a genetically engineered T-cell therapy in-house in its Division of Translational Immuno-Oncology.
For more information about this clinical trial, please call 1-800-767-9355.
Early August, 2017
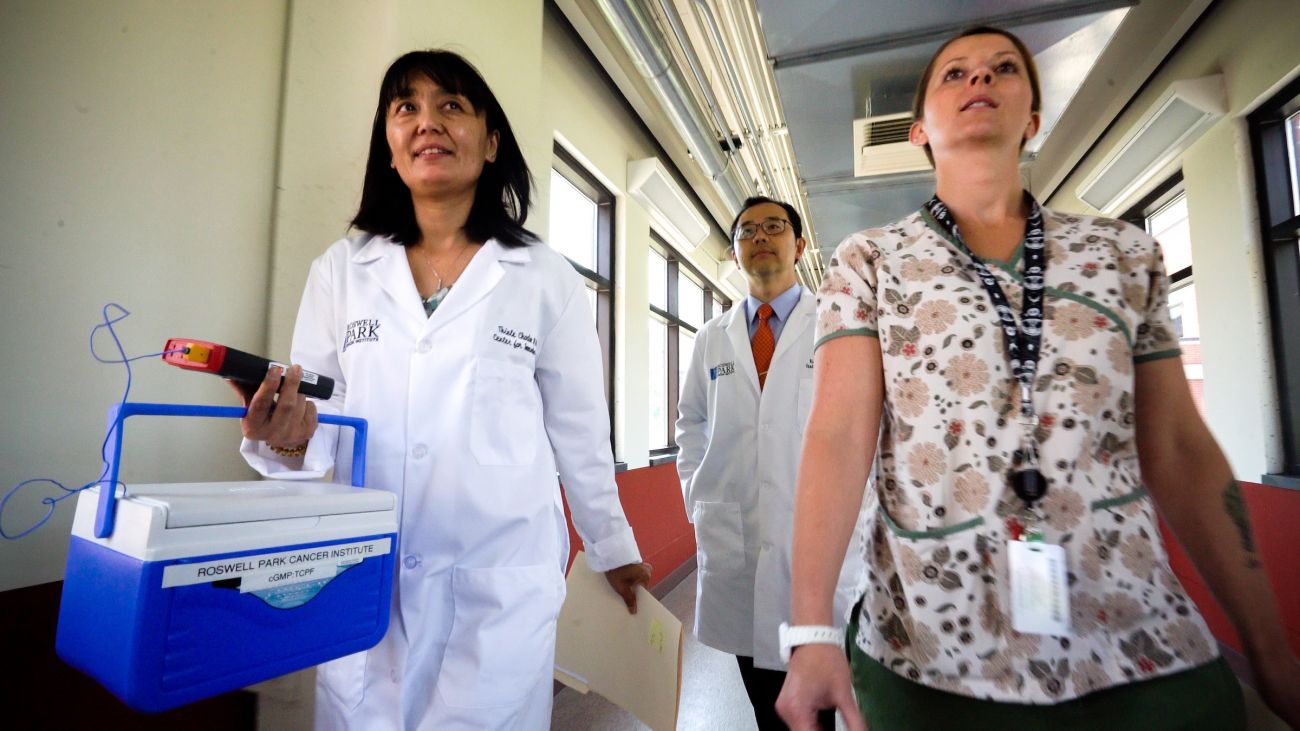
Thinle Chodon, MD, PhD, emerges from a lab in Roswell Park’s Division of Translational Immuno-Oncology carrying a small blue-and-white cooler. Inside, a plastic IV bag teems with 10 million disease-fighting T lymphocytes, or T cells — the frontline soldiers of the immune system.
Collected last week from a patient with late-stage ovarian cancer, these are not ordinary T cells; they have been altered and multiplied in the hope that when they are given back to her, they will launch a devastating attack on her cancer cells. Recently she underwent chemotherapy to destroy the weaker immune cells in her body, making room for the super-charged T cells that will take their place. Now everything is ready.
With three colleagues striding along beside her, Dr. Chodon heads quickly through the long hallways to the patient’s room in the Roswell Park hospital. Facility Director of the Division of Translational Immuno-Oncology’s Translational Research Operations, Dr. Chodon developed the procedures that were used to manufacture the T cells inside the IV bag and managed their production. She will be at the patient’s bedside during the infusion.
“First in Human”
The patient who is about to receive the cells is a pioneer. She will be the first person in the world to undergo this experimental treatment — a new and unique type of adoptive T-cell therapy developed at Roswell Park. Before coming here, she was treated at several other cancer centers, but surgery, chemotherapy, radiation therapy, and even a cancer vaccine could not halt the disease, which has now spread to her liver and lungs. No standard treatments are available for patients at this stage, and life expectancy is limited.
She could choose another treatment option — different chemotherapies, perhaps — but she has done her homework. After her original diagnosis, “I’d go to the computer and read journal articles,” she says. “I’d read and read, and I knew everything there was to know about cancer and ovarian cancer and treatments and classes of drugs.” And so she knows that standard chemotherapy is not likely to be effective against recurrent ovarian cancer.
“I started in a support group 10 years ago for women with my diagnosis. Now they’re all gone. They felt their best chances were to keep taking different [standard] treatments. It’s fear.
“But every single journal article you read on ovarian cancer starts like this: ‘The prognosis for ovarian cancer remains dismal,’ and then they give the statistics — this many cases, this many deaths. When is that going to change?
“By participating in this, I think in some way I’m helping humanity. But I also feel you can be self-centered and brave for your own ‘I want to live’ sort of thing. It’s a weird mix of all these different ideas that pushes you to do something like this.”
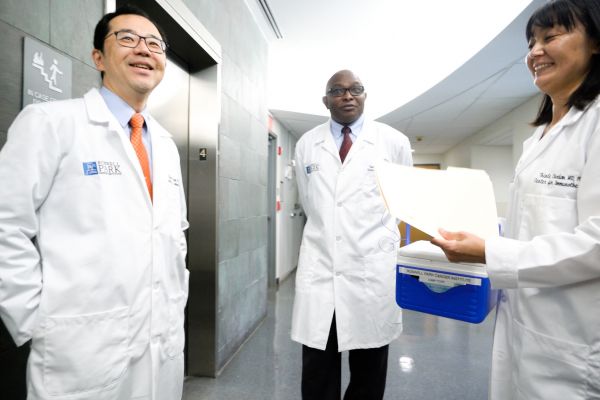
Scouring the National Cancer Institute website for information about upcoming clinical trials for which she might qualify, last winter the patient learned of an immunotherapy clinical trial that would soon open at Roswell Park. She traveled to Buffalo from out of state to meet with Kunle Odunsi, MD, PhD, formerly the Deputy Director of Roswell Park Comprehensive Cancer Center and Executive Director of the Division of Translational Immuno-Oncology. Together they discussed all her treatment options, including this clinical trial, for which Dr. Odunsi serves as Clinical Principal Investigator.
Participating in a “first in human” clinical trial can come with serious risks, the patient acknowledges. The treatment is unproven, so no one can predict the chances that it will have any effect on her cancer at all; in general, response rates to treatments offered in phase 1 clinical trials are low. But weighing her alternatives, she says, “I know my choice.”
Never miss another Cancer Talk blog!
Sign up to receive our monthly Cancer Talk e-newsletter.
Sign up!Day One
For every treatment now approved by the FDA, there was a Patient #1 — the first person to receive the treatment when it was experimental, when it first moved out of the laboratory to be tested in a human being. Today at Roswell Park, this woman becomes Patient #1.
Lying back in her hospital bed with a baseball cap covering her bald head, she is drowsy from a dose of Benadryl. Even amid the flurry of activity in her room — three doctors and four nurses crowd shoulder-to-shoulder around her bed — she keeps her eyes closed most of the time.
Laura Markel, RN, BSN, Clinical Nurse Manager, looks at the clock and announces, “We’re starting at 1:09.” The cells begin to flow from the bag into the patient’s arm.
Every two minutes during the infusion, Maureen Rogers, RN, calls out the patient’s blood pressure and respiration rate, keeping close watch in case of an unexpected reaction. Rogers holds the patient’s wrist gently, monitoring her pulse.
“You’re doing great!” Markel assures the patient.
“Thank you,” she replies softly, eyes still closed.
“How do you feel?”
“Fine.”
Ten minutes later, a beep alerts the nurses that the bag of cells is empty. Markel inspects the drip chamber and tubing, making sure no precious cells have been left behind.
“You did great,” she tells the patient.
That’s all for now. The next day, the patient is up and about, ticking off the dates she will return to Roswell Park over the next few weeks for blood work and monitoring. In six months, the first analysis will reveal whether her immune system has responded.
Before the end of the month, she is back at work, waiting and hoping.
To protect her privacy while the clinical trial is underway, Patient #1 is not identified in this article.
Stay tuned to Cancer Talk to learn about other clinical trials in the pipeline at Roswell Park’s Division of Translational Immuno-Oncology.
This is the first in a series of three Cancer Talk blogs about a new immunotherapy developed at Roswell Park.
Part 2: Roswell Park Hopes to Deliver Two-Pronged Attack on Cancer Cells through New Immunotherapy Approach
Part 3: The ABCs of Immunotherapy — and What's in the Pipeline at Roswell Park